Table of Contents
Rickets (osteomalacia)
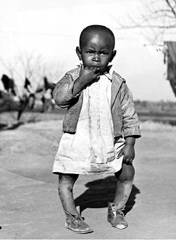
Rickets (osteomalacia) is a softening of the bones that leads to fractures and deformity. The majority of cases of rickets occur among children in developing countries who suffer from severe malnutrition. The disease is cited as a primary reason for consuming vitamin D regularly even though research has demonstrated that rickets is not caused by vitamin D deficiency but by hypophosphatemia.
The latest molecular evidence does not support adding high levels of vitamin D to the food chain in the name of “preventing rickets.” The health of the public would be much better served by regulations ensuring that they obtain adequate calcium and phosphorous rather than vitamin D.
Role of phosphorous
In a 2007 study, Harvard Medical School researchers engineered mice without vitamin D receptors (VDRs). Since vitamin D can have no effect on the body unless it can bind to the VDR, the mice could use no vitamin D whatsoever in their bodies. The researchers found that if the mice were given a diet high in calcium and phosphorous they did not develop rickets and their bones were just as strong as normal mice with active Vitamin D Receptors.1)
A second study by the same research team at Harvard corrected rickets by replacing calcium and phosphate ions in the bloodstream of mice without Vitamin D Receptors, thereby confirming the results. The team concluded that rickets is not caused by a deficiency of vitamin D but instead results from hypophosphatemia, a condition where the level of phosphorous in the blood is too low.2)
This work is also echoed by Schubert and De Luca who found that muscle weakness in hypophosphatemic rats could be corrected with supplementation of phosphorus, and that hypocalcemia together with vitamin D deficiency did not produce muscle weakness.3)
Role of calcium
According to a 2000 paper by Goswami et al., “Despite abundant sunlight, rickets and osteomalacia are prevalent in South Asian countries. The cause of this paradox is not clear.”4) Interestingly, the paper goes on to say that subjects who are at risk for rickets had low dietary calcium consumption and significantly low calcium consumption.
Along with phosphorous, low calcium plays a role in rickets. Diminished levels of calcium cause an increase in parathyroid hormone, which subsequently causes the body to excrete too much phosphorous. This causes the level of phosphate in the body to drop, leading to the altered bone formation seen in rickets.
Low phosphorus is the proximate cause — but low calcium intake is generally the ultimate cause.
Joyce Waterhouse, PhD
Other studies have confirmed that a low level of calcium can lead to rickets. One team assessed the absorption of calcium in 15 Nigerian children with active rickets. They found that all 15 children had resolution or improvement of rickets after six months of treatment with calcium supplements. 5)
This paper is acknowledged by the Children's Nutrition Research Center: Houston, TX
Interpretive Summary: Rickets in toddlers is a large problem in parts of Africa, especially Nigeria. It is not due to vitamin D deficiency but is caused by not having enough calcium in the diet. We wanted to know whether there was a problem with absorbing calcium in children in Nigeria. We measured how much calcium was absorbed in a group of children with rickets and compared that with how much was absorbed by children that did not have rickets. We found that children with rickets were able to absorb calcium normally. This means that it is probably another factor in the diet or an overall lack of calcium that causes the rickets rather than an inability of some children to absorb the calcium that is in their diet.
Vitamin D
The current prevailing view on vitamin D's role in rickets is epitomized by this 2008 statement:
Persons with a 25(OH)D3 concentration <20 nmol/L probably have rickets or osteomalacia.
Dr. Anthony Norman6)
However, a randomized double-blind placebo-controlled trial at Creighton University Medical Center found no beneficial effect of vitamin D on calcium absorption in older women.7)
Marshall Protocol patients
In fact, many of the patients on the Marshall Protocol have been avoiding consumption of vitamin D – some of them for several years – to the point where most patients in later stages of the treatment have 25-D levels below the detectable threshold. Yet, there has not been a single reported case of osteomalacia.
Louisianan infants
In 2010, Ponnapakkam et al. conducted a study to determine whether vitamin D supplementation should be required to prevent rickets in breast-fed infants. The study looked at both clinically apparent manifestations of rickets and and biochemical evidence of subclinical rickets.
We did not see any cases of rickets in any of the 80 study participants; as such, there was no evidence that universal supplementation of vitamin D in breast-fed infants is either necessary or efficacious for rickets prevention in southern Louisiana…. This suggests that the current recommendations for universal vitamin D supplementation of breast-fed infants throughout the United States may need to be revised.
Tulasi Ponnapakkam, PhD 8)
Nigerian children
Thacher et al conducted a case-control study to determine factors associated with rickets in Nigerian children. The study compared 123 Nigerian children who had rickets with matched control subjects. Of the 134 subjects with rickets, only 46 subjects (37%) had 25-hydroxyvitamin D values <30 nmol/L (12 ng/mL).9) The team concluded:
Vitamin D deficiency appears unlikely to be the primary etiologic factor of rickets in African children. Moreover, low dietary calcium intake alone does not account for rickets. Insufficient dietary calcium probably interacts with genetic, hormonal, and other nutritional factors to cause rickets in susceptible children.
Thacher et al. 10)
Molecular evidence
According to Marie Demay of Harvard Medical School, the lead author of a pair of recent papers on rickets:
We have no data that 1,25-D has any effect on the prevention of rickets…. Absence of ligand or receptor in the presence of normal mineral ions leads to a normal growth.
Marie Demay, personal communication
As a nod to this molecular evidence, the US Department of Agriculture has said, “Rickets in toddlers is a large problem in parts of Africa, especially Nigeria. It is not due to vitamin D deficiency but is caused by not having enough calcium in the diet.”
Does vitamin D have any role?
The USDA's conclusion (mentioned in the previous section) is consistent with common sense. It's hard to imagine that children in Africa, who get copious amounts of sunlight, which catalyzes vitamin D production, even in those with dark skin, are suffering from a disease caused by vitamin D deficiency.
If a child with rickets is severely deficient in vitamin D, as well as in calcium and phosphorous, administering a small amount of vitamin D (which will be immediately converted into 1,25-D) can help by allowing the Vitamin D Receptor to turn on genes that affect the absorption of calcium. This probably explains why in the early 19th century, some children given high does of vitamin D were said to be cured from rickets.
However, if supplementation is continued, the level of the precursor form of vitamin D (25-D) in the body will soon reach the point at which it becomes immunosuppressive. With the negative effects of this situation in mind, it makes much more sense that patients low in calcium should simply be given extra calcium, which can remedy the situation without the need for vitamin D.
Robins (2009) notes that nearly half of all African Americans are classified as vitamin-D deficient and yet show no signs of calcium deficiency, which would be a logical result of vitamin D deficiency. Indeed, they “have a lower prevalence of osteoporosis, a lower incidence of fractures and a higher bone mineral density than white Americans, who generally exhibit a much more favourable vitamin D status.” He also cites a survey of 232 black (East African) immigrant children in Melbourne, Australia, among whom 87% had levels below 50 nmol/L and 44% below 25 nmol/L. None had rickets—the usual sign of vitamin-D deficiency in children (McGillivray et al., 2007).
Peter Frost, PhD, African Americans and vitamin D
Reexamining the cause of rickets
The role of calcium is being reexamined in North America as well. DeLucia et al. emphasize that “Nutritional calcium deficiency may occur in North American infants and is not limited to the setting of developing countries.”11) Some attribute a recent small increase in rickets in North America to an increase in breast feeding, claiming that this is due to breast milk being low in vitamin D. However, breast feeding is also often accompanied by a diet low in calcium, particularly after weaning (e.g., juices rather than milk). Also, in recent years, more people have begun to avoid milk due to a greater awareness of lactose intolerance.
Trevor Marshall, PhD has suggested that rickets may be related to Th1 inflammation, as a number of patients on the Marshall Protocol with Th1 illnesses and their close relatives report having had rickets as children. Proponent of vitamin D supplementation claim that vitamin D added to the food supply was responsible for a historical decrease in rickets. But the history of rickets shows that a typical rickets case often had a history of smallpox, measles, or whooping cough.12) Plus, a 1997 study in Ethiopia found a high association between pneumonia and rickets.13) This provides more suggestive evidence that infection, either obvious and acute, or subtle and chronic, may play a role in the development of rickets and may exacerbate the effects of a low calcium diet.
Further reading
- ACE2 links amino acid malnutrition to microbial ecology and intestinal inflammation – In their 2012 Nature study, Hashimoto et al. provide a molecular explanation for how malnutrition promotes inflammation, “rogue” bacteria, and in the process diarrhea and other hallmarks of the condition.14)
[PMID: 17332234] [DOI: 10.1542/peds.2006-2023F]
[PMID: 16831920] [DOI: 10.1196/annals.1346.026]
[PMID: 20515645] [DOI: 10.1016/j.abb.2010.05.029]
[PMID: 10919943] [DOI: 10.1093/ajcn/72.2.472]
[PMID: 15531695] [DOI: 10.1093/ajcn/80.5.1415]
[PMID: 18689389] [DOI: 10.1093/ajcn/88.2.491S]
[PMID: 22855333] [PMCID: 3462946] [DOI: 10.1210/jc.2012-2020]
[PMID: 20724336] [DOI: 10.1177/0009922810376320]
[PMID: 10969262] [DOI: 10.1067/mpd.2000.107527]
[PMID: 12915633] [DOI: 10.1210/jc.2002-021935]
[PMID: 4862158] [DOI: 10.1093/ajcn/20.11.1234]
[PMID: 9269215] [DOI: 10.1016/S0140-6736(96)12098-5]
[PMID: 22837003] [PMCID: 7095315] [DOI: 10.1038/nature11228]