Table of Contents
Swollen lymph glands
Introduction
Lymph nodes play a criticial role in removing bacteria, abnormal cells and other matter as part of the immune system reaction to invasion by pathogens.
Lymphadenopathy (enlarged, swollen, or tender lymph nodes) is usually a sign of infection and is quite common in autoimmune diseases such as systemic lupus erythematosus, rheumatoid arthritis, and sarcoidosis. The |Wikipedia article on lymphadenopathy covers the range of causes. Note the distinction between infection and “autoimmuneA condition or disease thought to arise from an overactive immune response of the body against substances and tissues normally present in the body” disease, one which according to the Marshall PathogenesisA description for how chronic inflammatory diseases originate and develop., is trivial.
Lymphadenopathy can occur anywhere there are lymph nodes. Lymphadenopathy can often be detected by low-tech means: visually or by touch. Lymph nodes deep in the groin or beneath the ribs in the chest can be monitored with imaging such as chest x-ray, CT or PET scan.
Treating chronic disease with the Marshall ProtocolA curative medical treatment for chronic inflammatory disease. Based on the Marshall Pathogenesis. means that symptoms usually get worse before they get better, due to immunopathologyA temporary increase in disease symptoms experienced by Marshall Protocol patients that results from the release of cytokines and endotoxins as disease-causing bacteria are killed.. It is common for lymph nodes to increase in size, tenderness, and/or number as part of the immunopathology of recovery. This is evident when palpated or visible lymph nodes wax and wane with antibiotic administration. As the MP treats the underlying cause of sarcoidosis and lymphadenopathy, it may take many months for lymph nodes to return to normal size (reported to be 1 cm or less).
When one's doctor suspects enlarged lymph nodes may be cancer
In the case of sarcoidosis, most patients with lymphadenopathy had tests which ruled out lymphoma (cancer) before they were diagnosed with that illness.
Patients and doctors who do not understand the nature of immunopathology that occurs during the Marshall Protocol may become alarmed when lymph nodes increase in size or do not decrease. Doctors may want to reassure themselves or the patient by doing additional biopsies to, once again, rule out lymphoma. However, this invasive procedure is rarely necessary. Since lymphoma develops very slowly, a “watch and wait” tactic is more appropriate. Slowing down immunopathology or, if necessary, taking a break from the Protocol can also be done if anyone needs immediate reassurance that inflammationThe complex biological response of vascular tissues to harmful stimuli such as pathogens or damaged cells. It is a protective attempt by the organism to remove the injurious stimuli as well as initiate the healing process for the tissue. is responsible for emergent or increased lymphadenopathy while on the MP.
Patients experiences
[After an antibiotic break…] I am also happy to tell you all that the surgeon could not find the node it shrunk from 3.8cm to to small to safely do a punch biopsy. The vacation did it's job beautifully. The oncologist does not even want me for a follow up.
Hey this thing works.
Bill, MarshallProtocol.com
I was also concerned about the growth of my lymph nodes, as were my oncologist and pulmonologist, from December 2003-February 2004. They felt sure that I had lymphoma from the PET scan and the increased size and number found from numerous CT scans. The mediastinoscopy in February revealed the sarcoidosis. I had already begun Benicar; and after the surgery, I started the minocycline. The rest is history: The Marshall Protocol saved my life!
I had scans after surgery for three 3-month periods and then 6-month periods until last summer, which then became on a yearly basis. When I questioned several times about what “normal” would be, they said that it is usually anything 1 cm or less.
Carole, MarshallProtocol.com
Lumps were one of the big reasons I went to my doc for assistance. No-one seemed to be able to figure out what they were. After I met with my current doc he told me about the MP.
My lumps I think may be a mixture of enlarged lymph glands, lipomas, fat deposits.. .maybe granulomatous fibrosis or scarring. (?) Don't really know without a biopsy. I guess I've come to an uneasy acceptance that it doesn't matter….MP will hopefully address them all.
Well, during phase I and much of Modified Phase II, which I'm on now (approx 9 months total on MP) has seen an increase in lumps/lymph etc. Often these are very tender for a while, then eventually seem to become painless, though still enlarged or swollen. In the last month I have noticed that the chain of lumps/lymph on my right leg have truly begun to decrease. I didn't quite believe it at first as it was a very slow process. But they have absolutely become smaller….either getting softer and then fading away or getting smaller and becoming very hard, like the tip of a pin for sewing with those little knobs on top. Then, they seem to get absorbed. This has been SO reassuring to me. Even as I see that I may have more swellng/enlargement throughout MP, as I still am experiencing now in other parts of my body, I can feel reassured that there is a good chance they will eventually dissolve/be reabsorbed/melt away…whatever. Helps much with my anxiety about the whole thing, too. :)
SherryH, MarshallProtocol.com
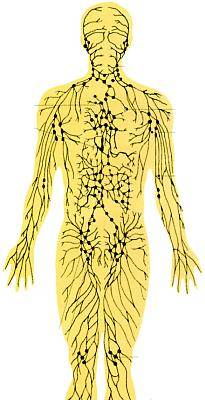
Lymphatic system diagram
Lymphatic drainage massage is done with gentle hand pressure moving very slowly from the furthest away body part toward the nearest nodes.
Research
pending