Table of Contents
Smoking tobacco
Smoking has been called “the single most preventable risk of disease” but the underlying disease process by which smoking is said to cause death and disease is not well-defined. However, there are several areas of study which point to the role of pathogens and modulation of the immune response in the diseases caused by smoking:
- Pathogens have been detected in cigarettes.1)
- Smoking has been shown to contribute to delayed apoptosis of immune cells as well as decrease production of antimicrobial peptides. Some evidence has emerged that smoking offers sick people symptomatic relief – through immunosuppression,2) an anti-inflammatory effect,3) or any number of other possible mechanisms.
- Sick people are less likely to quit smoking, which may artificially inflate estimate of the harmful effect of tobacco. For example, schizophrenic patients, have reported that they smoked “primarily for sedative effects and control of negative symptoms of schizophrenia.”4) Symptomatic relief may also explain why people with mental illness are twice as likely to smoke than people without a mental illness.5)
"The single most preventable risk of disease"
The World Health Organization estimates that tobacco caused 5.4 million deaths in 20046) and 100 million deaths over the course of the 20th century.7) Similarly, the United States Centers for Disease Control and Prevention describes tobacco use as “the single most important preventable risk to human health in developed countries and an important cause of premature death worldwide.”8)
Bacteria have been detected in cigarettes
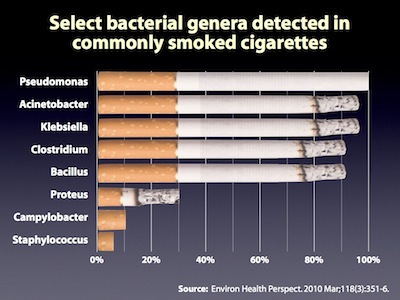
Compounds in cigarettes have been said to be carcinogenic. As discussed in Amy Proal's presentation at the 2010 International Congress on Autoimmunity, Sapkota et al. identified fifteen different classes of bacteria and a broad range of pathogenic organisms in five commonly smoked cigarettes tested.9) That said, the underlying disease process by which smoking is said to cause death is not well-defined.
Smoking is immunosuppressive
- Smoking and prolonged stress decrease production of antimicrobial peptides – Smoking and prolonged stress have been linked to increased susceptibility to bacterial infection. A 2010 study appearing in Cell Host and Microbe shows that this may be caused by a decrease in antimicrobial peptide (AmP) activity as a result of increased stimulation of a neuroendocrine signalling pathway.10) Radek et al. showed that when nicotinic acetylcholine receptors (nAChRs) were stimulated, mice had decreased AmP production and were increasingly susceptible to the pathogens methicillin-resistant Staphylococcus aureus and Group A Streptococcus infections.
- Nicotine interferes with apoptosis – According to a 2007 review, nicotine acts on immune cells. Although nicotine itself is usually not referred to as a carcinogen, there is ongoing debate whether nicotine functions as a “tumor enhancer.” By binding to nicotinic acetylcholine receptors, nicotine deregulates essential biological processes like angiogenesis, apoptosis, and cell-mediated immunity.11) Delayed apoptosis – that is, the inability of cells to self-destruct – is one of the hallmarks of chronic inflammatory disease. It is well-documented that microbes induce delayed apoptosis in order to gain a survival advantage.
Sick people are less likely to quit smoking
Though tobacco undoubtedly has some role in death and disease, the validity of these conclusions may not be as strong as some researchers have argued. Because conducting randomized controlled trials of tobacco users will likely never be conducted for ethical reasons, conclusions about tobacco must rely on certain statistical assumptions. Epidemiological studies of tobacco use multivariate analysis to control for any number of factors associated with likelihood of disease: education, age, ethnicity, income, gender, etc.
These types of studies assume that after controlling for all these key factors, people who smoke are statistically identical to people who don't smoke. But, epidemiological models may not fully account for the fact that people who are ill (or, especially people who are more likely to become ill) are more inclined to begin smoking, and more disinclined to discontinue smoking. Some evidence has emerged that smoking offers sick people symptomatic relief – through immunosuppression,12) an anti-inflammatory effect,13) or any number of other possible mechanisms.
Schizophrenic patients, for example, have reported that they smoked “primarily for sedative effects and control of negative symptoms of schizophrenia.”14) Symptomatic relief may also explain why people with mental illness are twice as likely to smoke than people without a mental illness.15) This effect may also be true for diseases which don't have a clear mental component.
If people smoke for symptomatic relief, there is a possible epidemiological paradox. As the health risks associated with smoking become more well-known, the less likely any given person is to smoke because of any reason but symptomatic relief. Under these circumstances, we would expect that the association between disease and smoking to increase in societies that begin to exert pressures (social, governmental, economic, etc.) against smoking.
This hypothesis deserves further exploration.
Smoking and Chlamydia pneumoniae
Smoking, an independent risk factor for cardiovascular disease, has also been shown to be an independent risk factor for C. pneumoniae seropositivity. It has also been suggested that an exacerbation of C. pneumoniae infection through smoking cigarettes may increase the potential for a systemic infection and therefore increase the chance for development of atherosclerosis.16)
Alternatives to smoking
Certain pharmaceutical preparations such as Nicorette gum contain nicotine for the treatment of tobacco dependence. Because as discussed above, nicotine appears to interfere with immune function,17) such smoking alternatives may impair patients' progress on the Marshall Protocol and are therefore contraindicated.
[PMID: 20064769] [PMCID: 2854762] [DOI: 10.1289/ehp.0901201]
[PMID: 9610683] [DOI: 10.1016/s0165-5728(97)00231-2]
[PMID: 12033743] [DOI: 10.1038/nri803]
[PMID: 12132630] [DOI: 10.1111/j.1744-6163.2002.tb00656.x]
[PMID: 20413096] [PMCID: 2916230] [DOI: 10.1016/j.chom.2010.03.009]
[PMID: 17846896] [DOI: 10.1007/s10495-007-0102-8]
[PMID: 10839723] [DOI: 10.1086/315602]
[PMID: 19244278] [DOI: 10.1093/toxsci/kfp044]