Related article: Olmesartan (Benicar) and kidney disease

This is an old revision of the document!
Table of Contents
Kidney (renal) function tests
Most patients on the MP experience temporary but well-defined increases in various markers of disease state and inflammationThe complex biological response of vascular tissues to harmful stimuli such as pathogens or damaged cells. It is a protective attempt by the organism to remove the injurious stimuli as well as initiate the healing process for the tissue., consistent with an immunopathological response. Results of blood tests for kidney function can generate considerable angst for Marshall ProtocolA curative medical treatment for chronic inflammatory disease. Based on the Marshall Pathogenesis. patients and their medical providers. Out of genuine concern for their patients, some physicians consider withholding prescription of olmesartanMedication taken regularly by patients on the Marshall Protocol for its ability to activate the Vitamin D Receptor. Also known by the trade name Benicar. . Experiences on the MP show that this concern may be mostly unfounded. And that the aberrant test values are to be expected from the nature of the MP treatment.
Doctors may want to assess kidney function by testing creatinine clearance test or BUN and measure other indicators specific to each patient for a baseline and retest as appropriate. Due to immunopathologyA temporary increase in disease symptoms experienced by Marshall Protocol patients that results from the release of cytokines and endotoxins as disease-causing bacteria are killed., lab these values may become temporarily abnormal until the inflammation resolves.
Measures of kidney function
- creatinine clearance (CrCl) – Measurement of the clearance of endogenous creatinine. The most valid test of kidney function. Compares the level of creatinine in urine with the creatinine level in the blood, usually based on measurements of a 24-hour urine sample and a blood sample drawn at the end of the 24-hour period
- creatinine – A break-down product of creatine phosphate in muscle, and is usually produced at a fairly constant rate by the body (depending on muscle mass).
- blood urea nitrogen (BUN) – A measure of the amount of nitrogen in the blood in the form of urea. urea is a substance secreted by the liver, and removed from the blood by the kidneys.
- glomerular filtration rate (GFR) – The volume of water filtered out of the plasma through glomerular capillary walls, which are located in the kidney. Best estimated by creatinine clearance test. The estimated value (eGFR) takes age, sex and race into account. Creatinine arising from ingested meat can raise blood levels to falsely lower eGFR.
Often MP patients will be told by their physicians they have a high BUN/creatinine ratio or high creatinine, which a physician may take to be an indication of kidney dysfunction. If this is concern, the physician may wish to order the creatinine clearance test, which is considered a more reliable indication of kidney function.
Olmesartan is renoprotective and has anti-inflammatory properties
Related article: Science behind olmesartan
Olmesartan has two key properties: Vitamin D Receptor agonistA substance such as olmesartan (Benicar) or 1,25-D which activates the Vitamin D Receptor and transcribes the genes necessary for a proper innate immune response. and potent anti-inflammatory. While it may seem logical to discontinue olmesartan given that it stimulates the immune response, leading to immunopathology and subsequently elevated kidney values, abruptly withdrawing olmesartan can be dangerous.
By reducing inflammation, olmesartan offers ongoing protection to the kidneys even while it is stimulating the VDRThe Vitamin D Receptor. A nuclear receptor located throughout the body that plays a key role in the innate immune response..1) 2) When the medication is discontinued, the patient's symptoms of disease can become significantly worse as olmesartan's anti-inflammatory protection is withdrawn. This is because while the drop in inflammation is immediate, the immune response which has been accelerated by olmesartan will continue to be strong even days, weeks, or months after discontinuing olmesartan.
Instead of discontinuing olmesartan, physicians are advised to work with their patients to employ one of several strategies to reduce the immunopathological response. Reducing, but not discontinuing entirely, antibiotics has often proven helpful.
If kidney values remain well above the acceptable range and olmesartan simply must be stopped, it is generally preferred to discontinue olmesartan gradually over the course of at least a couple weeks, and at any time except during an acute emergency.
The benefits of olmesartan on patients with kidney inflammation include:
- decreased insulin resistance, fewer symptoms of the metabolic syndrome, and decreased inflammation in patients with chronic kidney disease.3)
- the ability to ameliorate renal injury and fibrosis in rats when taken at ultrahigh doses.4)
- decreased (intra)renal vascular resistance, increased renal perfusion, and significantly reduced oxidative stress in patients with type 2 diabetes5)
- protection of the kidneys in diabetic nephropathy6)
- offer a survival benefit in hemodialysis patients, may help in preservation of renal function in predialysis patient, and affect the tissue repair process, reducing renal fibrosis7)
Recent studies of Olmesartan in patients
Increases in kidney metabolites on the Marshall Protocol
For MP patients with disease involvement in the kidneys, kidney-specific metabolites may increase in a way that is consistent with an active or activated immune response. The following research support this idea:
- BUN – One study found that hemodialysis patients who had high serum values of urea nitrogen (BUN) were less likely to have the acute infection, Helicobacter pylori.8) This suggests that temporary markers of kidney stress such as BUN may correlate with a robust and successful immune response.
- creatinine – According to Goldstein, clinicians caring for patients with acute kidney injury (AKI) have been hindered by the reliance on serum creatinine or decreased urine output, both kidney function markers, to make the AKI diagnosis. Even more vexing is the fact that similar serum creatinine changes can occur without kidney damage, for example in the context of dehydration, nephrotic syndrome or hepatorenal syndrome.9)
In a 2011 study appearing in Kidney International, Agarwal et al. gave 16 patients with chronic kidney disease daily doses of paricalcitol, an orally active vitamin D receptorA nuclear receptor located throughout the body that plays a key role in the innate immune response. (VDR) activator.10) (Note that the VDR plays a key role in innate immunityThe body's first line of defense against intracellular and other pathogens. According to the Marshall Pathogenesis the innate immune system becomes disabled as patients develop chronic disease..) The vitamin D analog was stopped after four days, and measurements were continued for three. During therapy, researchers found that subjects' serum creatinine significantly increased at a rate of 0.010 mg/dl/day and urine creatinine at a rate of 17.6 mg/day. Researchers also found a small increase in blood levels of BUN.
In conclusion, VDR activation may alter creatinine metabolism. An increase in creatinine generation may lead to an increase in serum creatinine and, if eGFR is used to measure kidney function, it may give the appearance that kidney function is declining when truly it may not be altered.
Rajiv Agarwal et al.11)
This work emphasizes the need for MP doctors to rely upon the 24-hour creatinine clearance test rather than eGFR to get the most accurate picture of real kidney function. Also, it validates the strategy of waiting-out abnormal creatinine values, rather than trying to intervene.
Patients experiences
As a matter of course, markers of kidney function including BUN and creatinine will fluctuate while a patient is on the MP. There is a tendency for some physicians to become alarmed by these fluctuations, particularly if a patient has kidney disease. However, for the vast majority of patients, these test results are an expected part of the healing process and will diminish over time.
Several patients have shown that measures of kidney function return to normal when they take measures (such as reducing antibiotics) to slow immunopathology.
I will have been off antibiotics for 25 days. My serum creatinine is now back down to 71 umol/L (0.81 mg/dL), with an eGFR of 80 mL/min. These are the same as before starting the MP, so my GP was “relieved” when I spoke to her this morning. I haven't been able to stop smiling all day!
Asilan, MarshallProtocol.com
Overall my health is mostly back to normal and I don’t notice any ill effects from these out of range kidney tests. However, as you can imagine, my Doc is quite alarmed. I have reviewed my 4 ½ year history with her (she is my third MP doc) and I have assured her that Benicar is renal protective, that it is normal for the kidneys to be loaded with toxins as the immune system eliminates the infection releasing toxins into the blood. And that this is proof, in fact, that the MP is working.
Measure Range 11/2007 4/2008 8/2008 9/2008 11/2008 4/2010 BUN (blood urea nitrogen) 7-25 24 30 (high) 32 (high) 18 40 (high) 35 (high) creatinine 0.5-1.3 1.3 1.2 1.59 (high) 1.23 1.54 (high) 1.57 (high) GFR (glomerular filtration rate) >60 44 (low) 59 45 (low) 44 (low) potassium 3.5-5.3 4.9 5 6.2 (high) 4.3 5.2 4.5 Gene Johnson, MarshallProtocol.com
Only Benicar every four hours during day time and a few times once at 3 a.m. My creatinine is down from 138 to 116 in a test taken two days ago (range 60-105). It was comforting to see that an increase in Benicar did not lead to an increase in creatinine as my nephrologist speculated it would.
Inge, MarshallProtocol.com
I received some good news during my doctor appointment. My kidney functioning tests were normal. My doctor had taken me off the MP meds back in May due to the increase in my creatinine and BUN. I wasn't sure how my tests results would be right now since I was now at the maximum doses of the MP meds. I was keeping my fingers crossed that the results would be good so my doctor wouldn't take me off the MP meds again. My doctor and I were both surprised to see that both my creatinine and BUN were normal.
Mike9a, MarshallProtocol.com
I'm now taking minocycline 25mg every two days Benicar 40mg every 3 to 5 hours. One week past “kidney crisis,” and new test results are almost normal. Whew.
Somadoc, MarshallProtocol.com
Comment
Creatinine level is an measure of activity, not a cause of damage (unlike v.D which is both a measure of, and cause of illness). Some researchers are considering its possible use as therapy
when used between 10–100 mM, suppression of growth and killing of all bacterial species were observed including not only drug-resistant strains, such as methicillin-resistant Staphylococcus aureus, but also uncharacterized environmental bacterial strains as well. The mechanism of action is as yet unclear.
Creatinine inhibits bacterial replication Thomas McDonald, Kristen M Drescher, Annika Weber and Steven Tracy 2012 12)
Notes and comments
- Legacy content
- f110:
This article talks about how bacteria can lead to release of nitric oxide: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC118062/
Blood Urea Nitrogen test is described here.
Simple explanation of alteration in kidney function tests while on the MP
A lot of MP patients get worried by low eGFR and highish creatinines, and experienced MP doctors know its not important.
Here's a short explanation which I hope helps to explain whats going on.
How to understand the relationship between serum creatinine, eGFR, and creatinine clearance:
Think of the serum creatinine level as a water level in a river. Its a spot measurement.
Think of the 24 hr creatinine clearance as the actual amount of water flowing down the river over 24 hours. This has been measured in your case.
Think of eGFR as a calculation or projection of the water flow, based on the spot measurement of the water level. This is highly inaccurate in certain circumstances, due to several important factors left out. The main assumption is that it never 'rains'.
But on the MP, the harder you herx, the more it 'rains'. So the water level (the serum creatinine) rises. But in most people on the MP, the river flow is not compromised at all (ie kidney function as measured accurately by 24 hr creatinine clearance) . We already know this intuitively because we know that its 'raining', ie that you are having high cell turnover and making a lot of creatinine due to herx. And we can know this deductively because you did a 24hr urine, and measured the amount of creatinine cleared in 24 hrs, which was completely normal.
So, when on the MP, serum creatinine and especially eGFR are really NOT showing what is going on. Much more important is 24 hr creatinine clearance. When 24 hr creatinine clearance is normal, then you know that you can ignore eGFR and serum creatinine, because they are only telling you how hard it is 'raining', and not how well your kidneys are functioning at all.
And those who do have real kidney impairment need to be checking 24 hr creatinine clearances and spot potassium levels. Potassium levels are very important to cardiac function, and high levels or low levels can trigger cardiac arrythmias.
Personally in most MP patients, I would more likely order a 24 hr creatinine clearance for a rising potassium level than a rising creatinine level on its own. Rising creatinine on its own needs to be managed as a sign of herxing, and managed by modulating the herxing in the usual way (increase olmesartan, adjust antibiotics etc).
I hope this helps you understand the numbers and what they do and do not represent.
Dr. Nyrie Dodd
http://www.medicalnewstoday.com/releases/231646.php
http://www.cell.com/cell-host-microbe/abstract/S1931-3128(11)00194-6
Cell Host Microbe. 2011 Jul 21;10(1):33-43. Multiple targets of nitric oxide in the tricarboxylic acid cycle of Salmonella enterica serovar typhimurium. Richardson AR, Payne EC, Younger N, Karlinsey JE, Thomas VC, Becker LA, Navarre WW, Castor ME, Libby SJ, Fang FC. Source Department of Laboratory Medicine, University of Washington, Seattle, WA 98195, USA. Abstract Host nitric oxide (NO⋅) production is important for controlling intracellular bacterial pathogens, including Salmonella enterica serovar Typhimurium, but the underlying mechanisms are incompletely understood. S. Typhmurium 14028s is prototrophic for all amino acids but cannot synthesize methionine (M) or lysine (K) during nitrosative stress. Here, we show that NO⋅-induced MK auxotrophy results from reduced succinyl-CoA availability as a consequence of NO⋅ targeting of lipoamide-dependent lipoamide dehydrogenase (LpdA) activity. LpdA is an essential component of the pyruvate and α-ketoglutarate dehydrogenase complexes. Additional effects of NO⋅ on gene regulation prevent compensatory pathways of succinyl-CoA production. Microarray analysis indicates that over 50% of the transcriptional response of S. Typhimurium to nitrosative stress is attributable to LpdA inhibition. Bacterial methionine transport is essential for virulence in NO⋅-producing mice, demonstrating that NO⋅-induced MK auxotrophy occurs in vivoA type of scientific study that analyzes an organism in its natural living environment.. These observations underscore the importance of metabolic targets for antimicrobial actions of NO⋅.
Copyright © 2011 Elsevier Inc. All rights reserved.
Comment in Cell Host Microbe. 2011 Jul 21;10(1):1-2. PMID: 21767810 [
It is not uncommon for creatinine levels to rise while having immunopathology during the MP. All of the usual methods for managing immunopathology should be employed.
The creatinine test is described here.
A good article to review is “Misconception #6: If my blood work (particularly that which pertains to kidney function) goes out of range after starting the MP, that’s a bad sign.” by Amy Proal.
Also, for more information, see Dr. Marshall's talk to doctors at West China Hospital, where he addresses this particular test.
Angiotensin-converting enzyme inhibitors and angiotensin receptor blockers: what to do if the serum creatinine and/or serum potassium concentration rises
“Elevations in serum creatinine with RAAS blockade: why isn't it a sign of kidney injury?” http://www.ncbi.nlm.nih.gov/pubmed/18695383
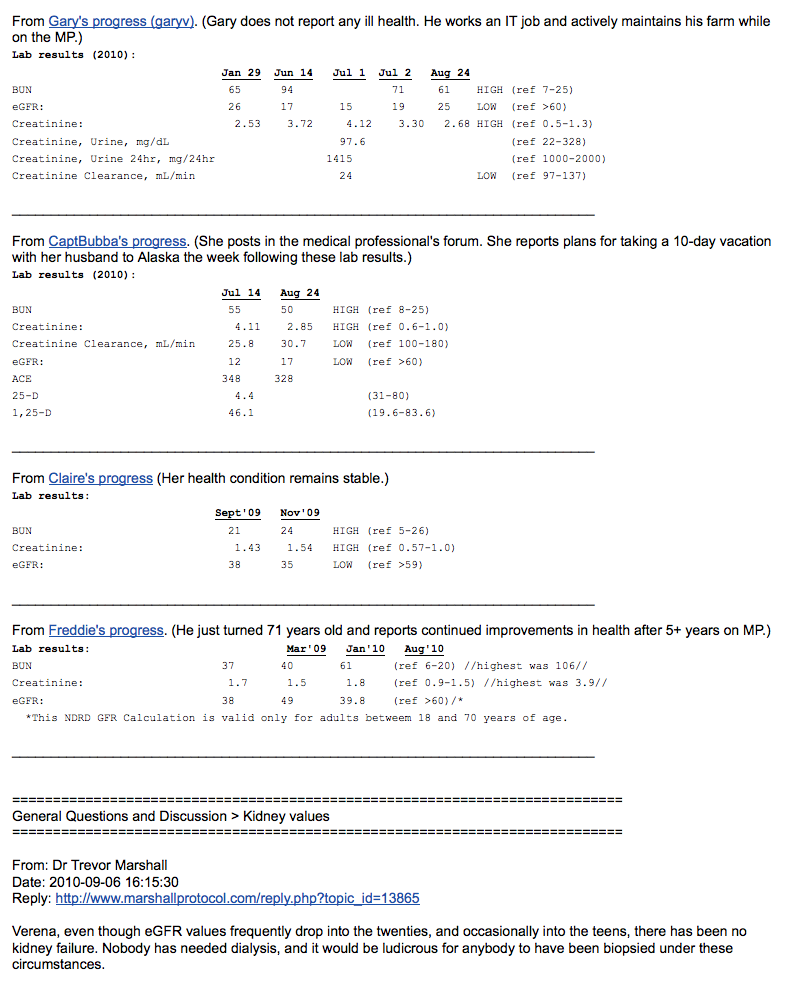
From Gary's progress (garyv). http://www.marshallprotocol.com/view_topic.php?id=12517&forum_id=35&jump_to=199982#p199982 (Gary does not report any ill health. He works an IT job and actively maintains his farm while on the MP.) Lab results (2010):
Jan 29 Jun 14 Jul 1 Jul 2 Aug 24
BUN 65 94 71 61 HIGH (ref 7-25) eGFR: 26 17 15 19 25 LOW (ref >60) Creatinine: 2.53 3.72 4.12 3.30 2.68 HIGH (ref 0.5-1.3) Creatinine, Urine, mg/dL 97.6 (ref 22-328) Creatinine, Urine 24hr, mg/24hr 1415 (ref 1000-2000) Creatinine Clearance, mL/min 24 LOW (ref 97-137)
From CaptBubba's progress. http://www.marshallprotocol.com/view_topic.php?id=12474&forum_id=17&jump_to=198938#p198938 (She posts in the medical professional's forum. She reports plans for taking a 10-day vacation with her husband to Alaska the week following these lab results.) Lab results (2010):
Jul 14 Aug 24
BUN 55 50 HIGH (ref 8-25) Creatinine: 4.11 2.85 HIGH (ref 0.6-1.0) Creatinine Clearance, mL/min 25.8 30.7 LOW (ref 100-180) eGFR: 12 17 LOW (ref >60) ACE 348 328 25-DThe vitamin D metabolite widely (and erroneously) considered best indicator of vitamin D "deficiency." Inactivates the Vitamin D Nuclear Receptor. Produced by hydroxylation of vitamin D3 in the liver. 4.4 (31-80) 1,25-DPrimary biologically active vitamin D hormone. Activates the vitamin D nuclear receptor. Produced by hydroxylation of 25-D. Also known as 1,25-dihydroxycholecalciferol, 1,25-hydroxyvitamin D and calcitirol. 46.1 (19.6-83.6)
_ From Claire's progress (Her health condition remains stable.) http://marshallprotocol.com/view_topic.php?id=8979&forum_id=35&jump_to=186714#p186714 Lab results: Sept'09 Nov'09 BUN 21 24 HIGH (ref 5-26) Creatinine: 1.43 1.54 HIGH (ref 0.57-1.0) eGFR: 38 35 LOW (ref >59) _
From Freddie's progress. (He just turned 71 years old and reports continued improvements in health after 5+ years on MP.) http://www.marshallprotocol.com/view_topic.php?id=5422&forum_id=35&jump_to=200005#p200005 Lab results: Mar'09 Jan'10 Aug'10 BUN 37 40 61 (ref 6-20) highest was 106 Creatinine: 1.7 1.5 1.8 (ref 0.9-1.5) highest was 3.9 eGFR: 38 49 39.8 (ref >60)/*
- This NDRD GFR Calculation is valid only for adults betweem 18 and 70 years of age.
___
General Questions and Discussion > Kidney values
From: Dr Trevor Marshall Date: 2010-09-06 16:15:30 Reply: http://www.marshallprotocol.com/reply.php?topic_id=13865
Verena, even though eGFR values frequently drop into the twenties, and occasionally into the teens, there has been no kidney failure. Nobody has needed dialysis, and it would be ludicrous for anybody to have been biopsied under these circumstances.
We have seen really high Creatinine, we should dig out these values and put them in the MPKB. I don't recall the values off the top of my head…
http://mpkb.org/home/protocol/olmesartan/kidney_disease
Hydration is important and harmless. We should be stressing this, and any other benign solutions (like oxygen for breathing difficulties).
Valsartan is only to be used to help people wean off the MP altogether. If we describe it in any other words we are asking for trouble. There is no evidence it can generally be used as a palliation by our brain-fogged members, even if it might help a few of the less seriously ill (see my previous email).
..trevor..
In certain cases, improved clinical outcomes are associated with elevated kidney metabolites. A recent Japanese four-year follow up study of 877 men found that lower serum creatinine was significantly associated with an increased risk of type 2 diabetes.13)
J Biomed Biotechnol. 2009;2009:284718. Epub 2009 Nov 1. Nitric oxide production by the human intestinal microbiotaThe bacterial community which causes chronic diseases - one which almost certainly includes multiple species and bacterial forms. by dissimilatory nitrate reduction to ammonium. Vermeiren J, Van de Wiele T, Verstraete W, Boeckx P, Boon N. Laboratory of Microbial Ecology and Technology (LabMET), Ghent University, Gent, Belgium. Abstract The free radical nitric oxide (NO) is an important signaling molecule in the gastrointestinal tract. Besides eukaryotic cells, gut microorganisms are also capable of producing NO. However, the exact mechanism of NO production by the gut microorganisms is unknown. Microbial NO production was examined under in vitroA technique of performing a given procedure in a controlled environment outside of a living organism - usually a laboratory. conditions simulating the gastrointestinal ecosystem using L-arginine or nitrate as substrates. L-arginine did not influence the microbial NO production. However, NO concentrations in the order of 90 ng NO-N per L feed medium were produced by the fecal microbiota from nitrate. (15)N tracer experiments showed that nitrate was mainly reduced to ammonium by the dissimilatory nitrate reduction to ammonium (DNRA) pathway. To our knowledge, this is the first study showing that gastrointestinal microbiota can generate substantial amounts of NO by DNRA and not by the generally accepted denitrification or L-arginine pathway. Further work is needed to elucidate the exact role between NO produced by the gastrointestinal microbiota and host cells. PMID: 19888436
- Vermeiren: Nitric oxide (NO), a free radical with moderate reactivity, has emerged as an important signaling molecule in a multitude of physiological systems in the human body [1]. In the gastrointestinal tract, NO is involved in the regulation of regional blood flow, smooth muscle relaxation, secretory and immunological regulation [2]. During inflammation the production of NO is induced. Rectal NO concentrations in healthy volunteers (range 3–25 ppbv) are significantly lower than the concentrations in patients with active inflammatory bowel disease (IBD) (range 71–8978 ppbv) [3]. NO can be synthesized in eukaryotic cells through oxidation of L-arginine by NO synthase (NOS) [4, 5]. Depending on the isoform of NOS catalyzing the reaction, nanomolar (endothelial NOS and neuronal NOS) or micromolar (inducible NOS) NO concentrations are produced serving as a messenger or as an antibacterial agent. Besides eukaryotic NO production, it is well known that NO can be produced also by microorganisms.
I have long been looking for a cite that explains how the destruction of bacteria results in increased BUN, because of production of nitric oxide. The attached paper comes pretty close. It says that NO can be produced by microorganisms.
It's interesting to me that this paper focuses on NO's role as a signaling molecule. Do you suspect that plays a significant role in MP patients' spike in BUN?
Paul
See Bruce Beutler's presentation - he considers both it and reactive oxygen species as signalling molecules (on one of his early LPS slides).
Patients experiences
-Have been to have my kidney function and BP checked and everything is much improved! Having increased my Benicar frequency to 6-hourly (and I've reduced my abx except mino to give my body a rest) my blood pressure has risen to a respectable 94/57. This is remarkable, as it had stabilized at 80/40 since I was in Phase 1. Creatinine, Urea, Urate and eGFR all returning to bearable levels. Only my anaemia remains but I will hope for that to improve slowly. So this is a lesson to others whose doctors panic and say “woah! your BP is dropping, you should take less of that Benicar”. The counter-intuitive answer is to TAKE MORE instead. ~Claudia
-My doc also worries about creatinine, but I never pushed for the 24hour test. What I did instead was to try to reduce herx, under the theory that creatinine was related to herx and both related to dying bacteria. What worked was to reduce the herx. It worked like a champ, my creatinine was normal.
What works to stop the herx seems to depend on the person and on the stage of MP. What works to convince a Doc that the Benicar isn't the problem is even more variable, but somehow you have to do it. ~Chris
-Finally my creatinine values are down in the normal range (101) (first time since I measured them in April). Hemoglobin is also up (11,5). Will slowly increase mino after having been to a nephrologist next week (only reason for seeing the specialist is to maintain a good relation to my doc). Think it is wise to keep creatinine low when I go see the specialist, so that no stopping of meds or anything will be enforced. Just finished a year on the MP, it has been a lot tougher than expected. And the time it takes seems so long. But hanging in there. ~inge 01/04/08
-I will have been off abx for 25 days. My serum creatinine is now back down to 71 umol/L (0.81 mg/dL), with an eGFR of 80 mL/min. These are the same as before starting the MP, so my GP was “relieved” when I spoke to her this morning. I haven't been able to stop smiling all day! ~Asilan
-I've had some blood tests back today and creatinine has gone down to 200. Potassium has gone down to 5.2. Urea has slightly gone down to 22.5. Haemaglobin and lymphocyte count are slightly low. So obviously slowing down the herx has helped with bloods. Bloods for me are a definite way of registering the herx because I'm always herxing and I'm not knowing the difference between tolerable and intolerable. Every since I took Benicar I found I was always herxing without the antibiotics and now I've been off Prednisilone for a year I feel like my immune reactions are very turned on and working stronger than when I started so I have found myself also dropping the antibiotic dose to cope with the herx. ~Simon
-I received some good news during my doctor appointment. My kidney functioning tests were normal. My doctor had taken me off the MP meds back in May due to the increase in my creatinine and BUN. I wasn't sure how my tests results would be right now since I was now at the maximum doses of the MP meds. I was keeping my fingers crossed that the results would be good so my doctor wouldn't take me off the MP meds again. My doctor and I were both surprised to see that both my creatinine and BUN were normal. ~Mike9a
-Mino 25mg every two days Benicar 40mg every 3 to 5 hours. One week past kidney“ crisis”: New test results are almost normal. Whew. ~Somadoc
-Just to let you know, that since stopping all abx and reducing the Beni to three times a day, things are much improved- as expected they would be. Kidney function: creatinine -89 ( was 103), eGFR =62 ( was 52). ~Kas
-only benicar every 4 hours during day time and a few times once at 3 am. creatinine down from 138 to 116 (two days ago) (range 60-105). it was comforting to see that an increase in benicar did not lead to an increase in creatinine, as my nephrologist speculated it would. ~inge
-the renal bloods are so much better & the Dr will no longer blame the Benicar for the abnormal readings. During all of that time I was on the 40mg q6h Benicar, plus the occasional 20mg. The creatinin seems to be going down & the eGFR up, towards the end of the zith cycle. ~Pundun
-My eGFR was retested at 53 up from 45 which my doc informally calls a percentage. Proof that decreased light and more Benicar increase it and therefore that it is IP :). ~PatrickBurke Jul08