Related articles: Anemia, Thyroid hormone and mineral supplementation
Table of Contents
Chronic fatigue syndrome (myalgic encephalomyelitis)
Introduction
Chronic fatigue syndrome (CFS) is the most common name given to a variably debilitating disorder or disorders generally defined by persistent fatigue unrelated to exertion, not substantially relieved by rest and accompanied by the presence of other specific symptoms for a minimum of six months. Other symptoms include musculoskeletal pain, sleep disturbance, impaired concentration, and headaches. New recognition for chronic fatigue Almost every aspect of CFS is the subject of disagreement and uncertainty1) – even diagnosis. There are no characteristic laboratory abnormalities to diagnose CFS,2) so testing is used to rule out other potential causes for symptoms. When symptoms are attributable to certain other conditions, the diagnosis of CFS is excluded.
Myalgic encephalomyelitis or chronic fatigue syndrome (ME/CFS) is a complex and debilitating disease of unknown etiology affecting more than one million Americans and millions of individuals worldwide (1, 2). ME/CFS is characterized by persistent or relapsing unexplained fatigue of at least 6-mo duration that is not alleviated by rest and results in a substantial reduction in previous levels of occupational, educational, social, and personal activities (2–5). In ME/CFS patients, fatigue is just one of multiple incapacitating symptoms that include cognitive impairment, postexertional malaise, unrefreshing sleep, headaches, myalgias, arthralgias, sore throats, lymphadenopathy, hypersensitivity to noise, light, or certain food items, and autonomic disturbances (4). These symptoms often cluster in each patient in varying combinations and intensity.3)
Surprisingly, conventional markers of inflammation commonly used in the daily practice of medicine (e.g., erythrocyte sedimentation rate, C-reactive protein) are seldom elevated in ME/CFS patients. Jose G. Montoya et al. July 2017 Proc Natl Acad Sci U S A.
The absence of well-defined biomarkers coupled with inability to point to a single somatic cause (e.g. an infectious process) has had a devastating effect on the way patients with CFS/ME are diagnosed, treated and regarded. Even though CFS/ME is now widely regarded as a “real” disease, the most popular explanation for this illness remains that it represents an extreme form of “medically unexplained illnesses.” As such, many psychiatrists have speculated that the condition is the product of maladaptive behaviors, failure to self-regulate, or any of dozens of others profoundly psychological or behavioral causes.4)
Three types of overlap occur among the disease states chronic fatigue syndrome (CFS), fibromyalgia (FM), multiple chemical sensitivity (MCS) and posttraumatic stress disorder (PTSD). They share common symptoms. 5)
An infectious etiology of chronic fatigue syndrome has long been suspected. Today, scientific evidence provides a growing, if not conclusive, link between infectious agents and CFS. For example, a 2011 study detected hundreds of unique proteins in the cerebrospinal fluid of patients with CFS as compared to healthy controls.
Presentation at the International Autoimmunity congress on the treatment of CFS with the Marshall protocol:
Contested name
Chronic fatigue syndrome (CFS) is the name currently used by the majority of the medical and scientific community to describe a condition or set of conditions characterized by fatigue and other symptoms. The term is contested, mostly by patients and patient advocacy groups, but also by some doctors. Several of the more common alternative names used to describe what most believe to be the same condition or subtypes include:
- myalgic encephalomyelitis (ME)
- chronic fatigue immune dysfunction syndrome (CFIDS)
- post-viral syndrome
- post-viral fatigue syndrome (PVFS)
- Gulf war syndrome
Hillary Johnson offers this partial history of the origin of the term “chronic fatigue syndrome”:
The illness became famous after an outbreak in 1984 around Lake Tahoe, in Nevada. Several hundred patients developed flu-like symptoms like fever, sore throat and headaches that led to neurological problems, including severe memory loss and inability to understand conversation. Most of them were infected with several viruses at once, including cytomegalovirus, Epstein-Barr and human herpesvirus 6. Their doctors were stumped. The Centers for Disease Control and Prevention, the nation’s presumed bulwark against emerging infectious diseases, dismissed the epidemic and said the Tahoe doctors “had worked themselves into a frenzy.” The sufferers, a C.D.C. investigator told me at the time, were “not normal Americans.”
When, by 1987, the supposed hysteria failed to evaporate and indeed continued erupting in other parts the country, the health agency orchestrated a jocular referendum by mail among a handful of academics to come up with a name for it. The group settled on “chronic fatigue syndrome” — the use of “syndrome” rather than “disease” suggested a psychiatric rather than physical origin and would thus discourage public panic and prevent insurers from having to make “chronic disbursements,” as one of the academics joked.
An 11th-hour plea by a nascent patient organization to call the disease by the scientific name used in Britain, myalgic encephalomyelitis, was rejected by the C.D.C. as “overly complicated and too confusing for many nonmedical persons.”
Had the agency done nothing in response to this epidemic, patients would now be better off. The name functioned as a kind of social punishment. Patients were branded malingerers by families, friends, journalists and insurance companies, and were denied medical care. (It’s no coincidence that suicide is among the three leading causes of death among sufferers.) Soon the malady came to be widely considered a personality disorder or something that sufferers brought upon themselves. A recent study financed by the C.D.C. suggested that childhood trauma or sexual abuse, combined with a genetic inability to handle stress, is a key risk factor for chronic fatigue syndrome.
Hillary Johnson, New York Times
However, CFS is a serious disease. The gentleness of its name barely suggests how debilitating the affliction is, and the use of the term “fatigue” diminishes the legitimacy of the illness. According to a survey of medical trainees at a school in the United States, a condition described as chronic fatigue syndrome may be considered less serious than a condition described as myalgic encephalopathy.6)
Diagnosis and testing
In the U.S., the most commonly used diagnostic criteria and definition of CFS/ME for research and clinical purposes were published by the United States Centers for Disease Control and Prevention (CDC).7) The Centers for Disease Control definition of CFS requires the following two criteria be fulfilled:
- A new onset (not lifelong) of unexplained, persistent fatigue unrelated to exertion and not substantially relieved by rest, that causes a significant reduction in previous activity levels.
- Four or more of the following symptoms that last six months or longer: impaired memory or concentration; post-exertional malaise, where physical or mental exertions bring on “extreme, prolonged exhaustion and sickness”; unrefreshing sleep; muscle pain (myalgia); pain in multiple joints (arthralgia); headaches of a new kind or greater severity; sore throat, frequent or recurring; tender lymph nodes (cervical or axillary).
There are no characteristic laboratory abnormalities to diagnose CFS/ME,8) so testing is used to rule out other potential causes for symptoms.9) When symptoms are attributable to certain other conditions, the diagnosis of CFS is excluded.
The absence of clear laboratory markers affects not only how CFS is diagnosed, but whether or not it is viewed as fundamentally psychological illness, and how it is treated.
Research
There is considerable evidence that mitochondrial dysfunction is present in some CFS patients. 10)
This work contributes key elements to the development of ME/CFS diagnostics, a crucial step required for discovering a therapy for any disease of unknown origin. 11)
Disturbances in fatty acid and lipid metabolism 12)
Selenium and iodine are essential for thyroid hormone synthesis and function. 13)
Altered composition of the gut microbiome 14)
A decisive infectious trigger may then lead to immunization against autoantigens involved in aerobic energy production and/or hormone receptors and ion channel proteins, producing postexertional malaise and ME/CFS, affecting both muscle and brain.15)
NK cells are a necessary component of the immunological process and aberrations in their functional processes, including equivocal levels of NK cells and cytotoxic activity pre-empts recurrent viral infections, autoimmune diseases and altered inflammatory responses. NK cells are implicated in a number of diseases including chronic fatigue syndrome (CFS)16)
Patients with CFS showed abnormalities in 20 metabolic pathways. 17)
Symptoms
Start by recognizing the symptoms. Here is an excellent description of life before diagnosis and the improvements possible once you know that the disease is not “all in the mind” and that real help exists.
Fatigue
Related articles: Fatigue, Stimulants
Patients with CFS may have levels of fatigue comparable to patients with late-stage AIDS.
My HIV patients for the most part are hale and hearty thanks to three decades of intense and excellent research and billions of dollars invested. Many of my CFS patients, on the other hand, are terribly ill and unable to work or participate in the care of their families. I split my clinical time between the two illnesses, and I can tell you if I had to choose between the two illnesses (in 2009) I would rather have HIV. But CFS, which impacts a million people in the United States alone, has had a small fraction of the research dollars directed towards it.
Nancy Klimas, M.D., New York Times
The systematic use of stimulants to manage symptoms of fatigue is not recommended.
Insomnia and poor sleep
Related articles: Insomnia and poor sleep, Sleep medications
The inability to sleep or sleep deeply is a common symptom of chronic inflammatory disease and can be exacerbated during periods of immunopathologyA temporary increase in disease symptoms experienced by Marshall Protocol patients that results from the release of cytokines and endotoxins as disease-causing bacteria are killed.. Restful sleep can help a patient to cope with other symptoms. It is not necessary to get all one's restful sleep at night. In fact, if a patient can, sleeping during the day may give him or her enough energy to accomplish any responsibilities for the day.
Cognitive dysfunction
Main article: Cognitive dysfunction
Cognitive dysfunctionThe loss of intellectual functions such as reasoning; memory loss; and other neurological abilities that is severe enough to interfere with daily functioning. (also known as brain fogThe loss of intellectual functions such as reasoning; memory loss; and other neurological abilities that is severe enough to interfere with daily functioning.) is the loss of intellectual functions such as thinking, remembering, and reasoning of sufficient severity to interfere with daily functioning. Patients with cognitive dysfunction have trouble with verbal recall, basic arithmetic, and concentration.
According to the Marshall PathogenesisA description for how chronic inflammatory diseases originate and develop., cognitive dysfunction is caused by microbes. More severe forms of cognitive dysfunction are seen in diseases such as Alzheimer's, diseases for which there is strong evidence of a bacterial etiology. Often associated with chronic fatigue syndrome,18) cognitive dysfunction is also seen in patients with multiple sclerosis,19) depression,20) fibromyalgia,21) and dozens of others diseases.
Like all symptoms of inflammatory disease, cognitive dysfunction may temporarily increase during periods of immunopathologyA temporary increase in disease symptoms experienced by Marshall Protocol patients that results from the release of cytokines and endotoxins as disease-causing bacteria are killed.. Cognitive dysfunction can be managed using the generic strategies for managing immunopathology, and should resolve over the course of the Marshall ProtocolA curative medical treatment for chronic inflammatory disease. Based on the Marshall Pathogenesis. (MP).
Some studies seem to suggest that sick women experience cognitive dysfunction more frequently and more severely than their male counterparts.22) 23)
Pain
Related articles: Pain, Pain medication and muscle relaxants
Related articles: Pain, Anesthetics for surgical procedures and allergic reactions
Pain is a symptom of Th1 diseaseAny of the chronic inflammatory diseases caused by bacterial pathogens. and can be exacerbated by immunopathologyA temporary increase in disease symptoms experienced by Marshall Protocol patients that results from the release of cytokines and endotoxins as disease-causing bacteria are killed.. Marshall ProtocolA curative medical treatment for chronic inflammatory disease. Based on the Marshall Pathogenesis. (MP) patients should always use 40mg of olmesartan (Benicar)Medication taken regularly by patients on the Marshall Protocol for its ability to activate the Vitamin D Receptor. every four hours, or more often, before resorting to pain medications. 20mg OLM under the tongue is quicker where pain is extreme.
There are also other strategies for managing pain.
When the usual strategies for managing immunopathology are not enough to control pain, some Marshall Protocol (MP) patients may need pain medications. Except for corticosteroidsA first-line treatment for a number of diseases. Corticosteroids work by slowing the innate immune response. This provides some patients with temporary symptom palliation but exacerbates the disease over the long-term by allowing chronic pathogens to proliferate., there is no pain medication contraindicated specifically because a patient is on the Marshall Protocol. Opioids are the preferred (short term) method of dealing with extreme pain in the MP cohort.
The effects of pain medications drugs on the immune system are not known. At present, it can't be said to what extent these drugs interfere with immunopathology. While it's strongly possible that some pain medications might temper immune system activity, patients taking them have made progress while taking them. As long as patients feel they're still experiencing immunopathology and that the medications are taken for reasons of necessity, pain medications are not contraindicated.
In conjunction with their physician or a pain management specialist, patients may want to experiment with different pain killers to see if any of them seem to lower not just pain but other disease symptoms. If they feel a particular pain medication is lowering immunopathology they are able to tolerate, they may want to ask their physician to change to a medication that does not elicit such an effect.
slowly I determined that caffeine, stress, and heat were triggers for all of my muscle spasms ..Internet article by MS sufferer
Exercise intolerance
Main article: Physical activity and exercise
For Marshall Protocol (MP) patients, the choice to exert oneself through physical activity or exercise should be made in the light of the stage of one's disease and the effect that extra activity has on the immune system. In different patients under different circumstances, exercise is capable of either suppressing or increasing the immune response.
MP patients who can perform their activities of daily living while recovering on the MP are as fit as they need to be. Their focus should be in regaining their health with the MP. With improved health will come improved abilty to exercise and increase endurance.
Cardiac problems
Related article: Managing cardiac symptoms
Related article: Cardiovascular diseases
The innate immune system response to microbes results in low-grade, often subclinical inflammationThe complex biological response of vascular tissues to harmful stimuli such as pathogens or damaged cells. It is a protective attempt by the organism to remove the injurious stimuli as well as initiate the healing process for the tissue. and chronic disease. Its effects can be seen in any part of the body including the heart. Treating chronic infections with the Marshall ProtocolA curative medical treatment for chronic inflammatory disease. Based on the Marshall Pathogenesis. (MP) unavoidably results in increased inflammation. While a severe cardiac immunopathological reactionA temporary increase in disease symptoms experiences by Marshall Protocol patients that results from the release of cytokines and endotoxins as disease-causing bacteria are killed. is rare, it has the potential to be life-threatening. Therefore, health care providers are cautioned to be on the alert for cardiac symptoms in all their patients. Also, patients with risk factors should know when seek medical attention.
Physicians and patients anticipating strong cardiac immunopathologyAn exacerbation in symptoms of the heart muscle. Requires careful management by physicians. should also review these documents:
- Notice for emergency medical personnel – for health care providers treating a Marshall Protocol patient in an emergency situation
Respiratory problems
Main article: Managing respiratory symptoms
Metabolic evidence
As reported in The Economist “ Robert Naviaux of the University of California, San Diego, and his colleagues published evidence24) that the metabolisms of those diagnosed with CFS are all changing in the same way.”
in 2016, “Dr Naviaux and his team collected and analysed blood samples from 45 people who had been diagnosed with CFS, and also from 39 controls who were free of any CFS-related symptom. They then trawled through those samples looking at the levels of 612 specific chemicals, known as metabolites, which are produced during the day-to-day operations of living cells.
These metabolite profiles, they found, differed clearly and systematically between the patients and the controls. Some 20 metabolic pathways were affected, with most patients having about 40 specific abnormalities. The biggest differences were in levels of sphingolipids, which are involved in intercellular communication, though other molecules played a role as well. These differences should give clues as to what is happening at a cellular level during CFS. More immediately, a handful of the abnormalities—eight in men and 13 in women—were enough, collectively, to diagnose with greater than 90% accuracy who had the disease.”
Evidence of infectious cause
Today scientific evidence may provide a link between infectious agents and Chronic Fatigue Syndrome.
In October 2009, we reported the first direct isolation of infectious xenotropic murine leukemia virus-related virus (XMRV). In that study, we used a combination of biological amplification and molecular enhancement techniques to detect XMRV in more than 75% of 101 patients with chronic fatigue syndrome (CFS).25)
Impairment of immune function
Mingli Liu, et al, CytokineAny of various protein molecules secreted by cells of the immune system that serve to regulate the immune system. Growth Factor Rev. 2011 Jun; 22(3): 121–130.
C-X-C motif chemokine 10 (CXCL10) also known as interferon γ-induced protein 10 kDa (IP-10) or small-inducible cytokine B10 is a cytokine belonging to the CXC chemokine family. CXCL10 binds CXCR3 receptor to induce chemotaxis, apoptosis, cell growth and angiostasis. Alterations in CXCL10 expression levels have been associated with inflammatory diseases including infectious diseases, immune dysfunction and tumor development. CXCL10 is also recognized as a biomarker that predicts severity of various diseases. A review of the emerging role of CXCL10 in pathogenesis of infectious diseases revealed diverse roles of CXCL10 in disease initiation and progression.
Environmental issues
wireless signals can interfere with living systems
This past year we have identified and begun to document the impairment of immune function caused by the massive global build-out of wireless technologies.
Something as simple as a wireless home telephone can cause all the symptoms of CFS/ME in people. Symptoms that often resolved when the wireless home phone was removed. Unfortunately, there are also wireless signal sources that are coming into many homes that can't be removed by us (cell towers, neighbor's wi-fi, etc.)
Joyful 2015
History of conflicting results
Related articles: Detecting bacteria, Koch's postulates
An infectious etiology of Chronic Fatigue Syndrome has long been suspected and investigated, often with inconsistent results.26) 27) The debate over whether XMRV, EBV, or any other single pathogen causes CFS reflects an over-reliance on the antiquated model of disease set forth by Koch's postulates – namely that a pathogen must be: found in all cases of the disease examined, prepared and maintained in a pure culture, capable of producing the original infection, even after several generations in culture, and retrievable from an inoculated animal and cultured again. For all their lingering influence, Koch's postulates never anticipated the era of the human metagenome in which thousands of difficult or impossible-to-culture species of bacteria – rather than just one – contribute to a single disease state.
Different proteins in cerebrospinal fluid
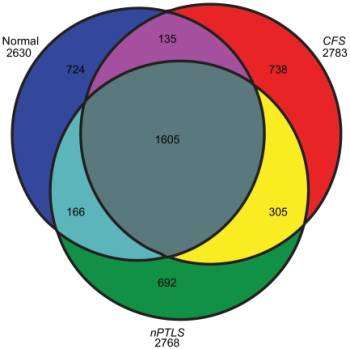
In a 2011 study appearing in PLoS One, Schutzer and colleagues analyzed spinal fluid samples from three groups — 11 healthy people, 43 diagnosed with chronic fatigue syndrome and 25 previously treated for Lyme disease but who were still experiencing cognitive problems and fatigue.28) Analysis of the fluid samples detected more than 2,600 proteins in each group. Most of the proteins appeared in all three groups. But 692 proteins turned up only in the Lyme patients and 738 others showed up only in the chronic fatigue group.
On its most basic level, this study offers strong evidence of a biological component for Lyme and CFS. The presence of so many unique proteins suggests that these are proteins are either created directly by microbes or are the results of microbes acting on the human genome.
In the aftermath of the study, several commentators have noted that this work could be built upon to more definitely distinguish Lyme from CFS. However, it is interesting to note that a significant number of proteins are common to both CFS and Lyme. The reductionist approach, in which a disease state is defined by a single or even a handful of proteins may not fully account for the complexity of human microbiome and the nature of the disease process.
EBV
In the late 1980s and early 1990s, EBV became the favored explanation for chronic fatigue syndrome. It was noted that people with chronic exhaustion had EBV, although it was also noted EBV was present in almost everyone. In a four year study, the Centers for Disease Control and Prevention found that the virus did not adhere to Koch's postulates and therefore had no definitive association between CFS and EBV but it is still being studied by researchers.
XMRV
In 2009, researchers published a paper in the journal Science announcing that in 67% of the samples of 101 chronic fatigue syndrome patients (as compared to 3.7% of 218 healthy controls), they had found a retrovirus called XMRV: xenotropic murine leukemia virus-related virus.29) However, numerous other labs trying to duplicate the results of the Science paper were unable to find the retrovirus in patients with the disease.30) In the wake of recent studies,31) editors for the journal Science have gone so far as to ask the original authors to retract their paper.32)
For many scientists, the inability of other labs to confirm the results raised questions about the validity of the retroviral finding. Others such as W. Ian Lipkin have suggested that other factors may be to blame: varying definitions of CFS could contribute to conflicting reports, as well as differences in the way labs process blood samples, and which tests they use.
Enterobacteria and enteroviruses
A number of studies have detected enterobacteria in the gut of patients with CFS. Maes et al. found that the prevalences in response to the presences and median values for serum IgA against the lipopolysaccharides of enterobacteria are significantly greater in patients with CFS.33) The presence of chronic disseminated enteroviral infection, as determined by stomach or muscle biopsy, has also been identified in a subset of patients with the syndrome. Acquisition of these pathogens as part of the successive infectionAn infectious cascade of pathogens in which initial infectious agents slow the immune response and make it easier for subsequent infections to proliferate. process may well contribute to common CFS “comorbidities” such as irritable bowel syndrome or sensitivities to certain foods.
Chronic fatigue syndrome is associated with chronic enterovirus infection of the stomach.34)
Mycoplasma
Nijs et al. found a high prevalence of Mycoplasma infections among European chronic fatigue syndrome patients.35) In this prospective study, the presence of Mycoplasma fermentans, M. penetrans, M. pneumoniae and M. hominis was assessed in the blood of 261 European CFS patients and 36 healthy volunteers using forensic polymerase chain reaction. One hundred and seventy-nine (68.6%) patients were infected by at least one species of Mycoplasma, compared to two out of 36 (5.6%) in the control sample. Multiple mycoplasmal infections were detected in 45 patients (17.2%). Compared to American CFS patients (M. pneumoniae > M. hominis > M. penetrans), a slightly different pattern of mycoplasmal infections was found in European CFS patients (M. hominis > M. pneumoniae, M. fermentansz & M. penetrans).
Other infections
Certain other infectious illnesses, such as Q fever and viral meningitis are associated with a greater risk of developing CFS, but many people have no evidence of viral infection, and there is no evidence of persistent infection.36)
Incline Village and other outbreaks
There are several reports of CFS outbreaks, one prominent example of which is Incline Village.
[The] clusters of post-infectious chronic fatigue syndrome are very interesting. Studies by Andrew Lloyd and colleagues37) showed the one and only predictor of persistent illness after an acute infection was the severity of that initial infection. No psychiatric factors were shown to predict who remains ill.
Some very common infections seem to set off C.F.S. and lead to several theories about the disease. My favorite theory is that any infection that can activate the immune system in a profound way could allow a hidden latent virus or viruses to reactivate and perpetuate a chronic illness. Anything that suppresses the immune system, like some treatments for cancer, might do the same thing, causing profound fatigue in some “recovered” cancer patients years after chemotherapy.
Nancy Klimas, M.D., New York Times
Length of the MP
Main article: Length of the Marshall Protocol
The length of time it takes an MP patient to return to a given level of functionality seems to vary somewhat by disease. Diseases like CFS and Lyme are likely to take longer. This may be because patients with these diseases tend to be sicker than most.
I think that, in general, CFS and Lyme patients have had more long-term intervention from supplements and pharmaceuticals than many of the sarcies. Additionally, their disease is not as apparent as, for example, lupus or sarcoidosis, and this means that they generally are more ill before they get help. A sarc patient, for example, may die of pulmonary insufficiency or cardiac arrest before their overall systemic organ status degenerates to that of some of the CFS and Lyme patients.
I don't think there is any fundamental difference in the species, however. I myself suffered from debilitating fatigue for almost a decade, and had to work my life around my unusual sleep and rest patterns. It was seeing that fatigue in the diabetes patients (whom I was researching) that first made me realize the common threads through all the Th1 diseasesThe chronic inflammatory diseases caused by bacterial pathogens..
I do think it is important that CFS and Lyme patients do face up to the extent of their illness, however. Think about this - it takes 2 years or more for the bacteria to be killed, at the fastest rate your body can kill them. It is absolutely amazing what that quantity of bacteria must have been doing while they were living in your tissues
Trevor Marshall, PhD
Data
from DJ in California During the summer of 2013 I looked at 2,000 records of people using the Marshall Protocol.
I eliminated all records that had less than 20 messages, as these were usually inquiries into the treatment without actual participation. I eliminated all records from people who had been banned from the site. I eliminated all records from Health Professionals who did not actually have disease. I eliminated all records where I could not find a valid progress report. This left me with 864 meaningful records.
I tried my best to be unbiased as I was expecting to see about a 20% improvement in health of members, or in other words a 20-25% success rate. I was intending to compare this to the 10% success rate I found done on the use of prednisone to treat Sarcoidosis. That double blind report shows that 10% treated with prednisone achieve remission. (BTW remission in Sarcoidosis as far as I can find out is measured rather subjectively) The following information is what I found:
Chronic Fatigue Syndrome: 183 members; 110 success; 30 no success; 43 unsure
TOTALS: 864 members;573 report success; 119 report no success; and for 172 results are not clear.
SUCCESS RATES: Over all success rate 66.32% Over all unsuccessful 13.77% Over all unsure 19.91%
Chronic Fatigue Syndrome success 60.1%
All Other Th1 disease success 59.8%
What we who are a part of this forum, who stuck with the protocol long enough, who endured the IP and were able to keep a doctor, report is that this has a better than 50% success rate.
Cognitive, behavioral and psychosocial explanations
Related article: Psychosomatic explanations for disease
Sigmund Freud and Jean-Martin Charcot were born 150 years ago, but their ideas about the effect of the subconscious on disease continue to resonate in the scientific community.38) Freud and colleagues argued that unconscious mental processes such as sublimated rage could manifest as physical symptoms. However, with the advent of superior technology, one by one, many diseases once supposed to be caused by psychological stress have since been attributed to other factors including infections.
According to the Marshall Pathogenesis, chronic fatigue syndrome, multiple chemical sensitivity and other chronic inflammatory diseases are likely caused by pathogens, yet many physicians consider these diseases to be “medically unexplained.” Medically unexplained diseases are widely prevalent39) but at the same time have few discernible markers or objectively measurable symptoms. While a lot of Freudian ideas have fallen out of favor, one legacy remains: difficult-to-explain diseases are still routinely attributed to psychological causes. The process by which patients supposedly manifest psychological problems as a disease has been named and renamed, classified and reclassified: hysteria, psychosomatic disorder, somatoform disorder, conversion disorder, functional disorder, etc. In each of these diagnoses, however, the stated origin of disease is unchanged: symptoms that cannot be explained are ultimately “all in a patient's head.”
While there is no denying the existence of some sort of “mind-body connection,” there is minimal compelling evidence that as the 19th century Swiss physician Georg W. Groddeck claimed: “Illness has a purpose; it has to resolve the conflict, to repress it, or to prevent what is already repressed from entering consciousness.”40) Despite the stark absence of evidence supporting these views, it is not unusual to read papers describing how patients with long-term so-called psychological illnesses may be subconsciously manifesting them, because it would allow them to have more “care, attention, disengagement, or even financial benefits.”41) Nor, is it uncommon for new theories to spring up along these lines. In one example, a 2008 continuing medical education publication taught physicians that when a celebrity becomes ill, healthy people are suggestible enough to develop long-term illnesses consistent with the celebrity's descriptions of their conditions. Such claims are recklessly speculative, harming patients and stalling needed research.
Treating patients who complain of so-called medically unexplained symptoms with cognitive behavioral therapy or, in the case of chronic fatigue syndrome, graded exercise therapy, may do more harm than good.42) The emergence of metagenomic technologies offers a more sophisticated set of tools for detecting and characterizing microbes in these disease states. Perhaps it is only the use of this technology that will finally relegate the notion of patient as attention-seeking victim to historical relic.
Behavioral explanations
CFS/ME patients' behaviors are routinely blamed for causing, if not driving, their illnesses, because they:
- unnecessarily seek medical care – One study found CFS patients consulted their physician more frequently in the 15 years before development of their condition.43) This study proves only that CFS patients had signs of sickness (and noticed them) prior to diagnosis.
- participate in social networks – A lack of support or the reinforcement of “illness behaviour” by social networks has been proposed to delay recovery for some patients.44)
- display high levels of “action-proneness” – Van Houdenhove et al. employ this euphemism for saying patients were “hyperactive” prior to disease onset.48) 49) This is analogous to claiming patients with obstructive lung diseases contract those illnesses by excessive breathing. According to this logic, unlike nearly every other disease, patients' dissatisfaction with being sick is responsible for them remaining sick.
- engage in catastrophizing – A euphemism for fearing the worst.50)
Cognitive explanations
According to a 2006 Lancet paper, “Inactivity of patients with CFS is caused by perceptions and expectations rather than by physical fitness.”54) Patients with the condition supposedly:
- perceive symptoms inaccurately – Prins summed up the literature when she said there are discrepancies between perceived and actual cognitive performance, perceived and actual sleep disturbance, and perceived and actual functioning.55)
- are neurotic and introverted58) – However, a more recent systematic review of personality and CFS found an association with neuroticism, but stated that it was often accounted for by co-morbid depression and levels were similar to those in patients with other chronic diseases, and found no firm evidence for introversion.59)
- fail to self-regulate – Deary has hypothesized that in CFS/ME, the health threat is no longer the illness, but anything that threatens to disrupt a precarious accommodation to it.60) Due to established vicious circles, attempts at threat regulation may become inadvertently self-defeating, promoting the threats they attempt to diminish. By logical extension, CFS/ME patients who dismissed this argument would do so because they are sick and in so doing, continue to be sick. Or, in other words, failure to agree with a researcher's belief about an illness causes that illness.
- engage in somatization – So called “somatoform diseases,” are conditions in the which internal psychological conflicts are unconsciously expressed as physical signs has also been implicated.61)
Therapy based on the cognitive-behavioral model of disease
Cognitive behavioral therapy (CBT), graded exercise therapy (GET) and other interventions for CFS/ME are predicated on the profoundly flawed cognitive-behavioral model for the disease. They also suffer from bias. For example, because many of the CBT and GET studies required patients to visit a clinic, severely affected patients may have been excluded.62)
- cognitive behavioral therapy – CBT is a form of psychological therapy in which patients are taught to solve problems concerning dysfunctional emotions, behaviors and cognitions through a goal-oriented, systematic procedure. Being chronically ill can be very challenging, and professional counseling for diseases that have profound neurological components, is usually useful. But the whole point of this therapy is to “help” the patient develop behaviors and insights into why they are ultimately responsible for their illnesses.
- graded exercise therapy – GET is a form of physical therapy in which patients being exercising very slowly and gradually increase exercise duration and intensity over time.
Because patients suffering from CFS/ME suffer from an organic cause, these interventions are unsettling, if not sadistic. It is tragic or humorous to think either therapy would ever be considered a first-line therapy for illnesses such as AIDS, leprosy or other diseases for which the infectious causes of which are less disputed.
We conclude that it is unethical to treat patients with ME/CFS with ineffective, non-evidence-based and potentially harmful “rehabilitation therapies”, such as CBT/GET.
F.N. Twisk, et al.63)
As of November 2010, the top three treatments for CFS on the CDC website remain, respectively: professional counseling, cognitive behavioral therapy (CBT), and graded exercise therapy (GET).
Other treatments
- Rituximab – In 2011, a Norwegian study published in PLoS One studied the effect of Rituximab – a monoclonal antibody otherwise used in cancers and anti-rejection treatment for organ transplants – on patients with CFS. In the 25-week study period, fatigue improved significantly in 10 out of 15 patients versus 2 out of 15 controls.64) This positive result may be due to the fact that Rituximab is a strong immunosuppressant. It may be telling to see a follow up of the patients who received the drug ten or even fifteen years from now.
Patient interviews



autism, ADHD, depression, severe anxiety, chronic fatigue syndrome (CFS)
Read the interview

Unrest - Documentary on ME
Interviews of patients with other diseases are also available.
Read more
- A case of chronic denial – New York Times editorial written by the author of Osler's Web
- Osler's Web: Inside the Labyrinth of the Chronic Fatigue Syndrome Epidemic – a thorough medical and political history of this decades-old (and variously named) syndrome during the epidemic years of 1984-1994
Recent research
Montoya et al. July 2017 Proc Natl Acad Sci U S A65)
To determine whether a signature of serum cytokinesAny of various protein molecules secreted by cells of the immune system that serve to regulate the immune system. could be associated with ME/CFS and correlated with disease severity and fatigue duration, cytokines of 192 ME/CFS patients and 392 healthy controls were measured using a 51-multiplex array on a Luminex system. Each cytokine’s preprocessed data were regressed on ME/CFS severity plus covariates for age, sex, race, and an assay property of newly discovered importance: nonspecific binding. On average, TGF-β was elevated (P = 0.0052) and resistin was lower (P = 0.0052) in patients compared with controls. Seventeen cytokines had a statistically significant upward linear trend that correlated with ME/CFS severity: CCL11 (Eotaxin-1), CXCL1 (GROα), CXCL10 (IP-10), IFN-γ, IL-4, IL-5, IL-7, IL-12p70, IL-13, IL-17F, leptin, G-CSF, GM-CSF, LIF, NGF, SCF, and TGF-α. Of the 17 cytokines that correlated with severity, 13 are proinflammatory, likely contributing to many of the symptoms experienced by patients and establishing a strong immune system component of the disease. Only CXCL9 (MIG) inversely correlated with fatigue duration.
Comparison of mean cytokine levels (pMFI) in ME/CFS patients
Chronic fatigue syndrome patients have alterations in their oral microbiome composition and function. 66)
[PMID: 16835542] [DOI: 10.12968/bjon.2006.15.12.21399]
[PMID: 14702202] [PMCID: 317472] [DOI: 10.1186/1472-6963-3-25]
[PMID: 28760971] [PMCID: 5576836] [DOI: 10.1073/pnas.1710519114]
[PMID: 18267050] [DOI: 10.1348/135910708X283760]
[PMID: 11461161] [DOI: 10.1054/mehy.2001.1325]
[PMID: 11928774] [DOI: 10.1023/A:1014328319297]
[PMID: 12562565] [DOI: 10.1176/appi.ajp.160.2.221]
[PMID: 7978722] [DOI: 10.7326/0003-4819-121-12-199412150-00009]
[PMID: 19436827] [PMCID: 2680051]
[PMID: 30563204] [PMCID: 6315598] [DOI: 10.3390/metabo8040090]
[PMID: 28059425] [PMCID: 5365380] [DOI: 10.1039/c6mb00600k]
[PMID: 26088475] [DOI: 10.2174/1871530315666150619094242]
[PMID: 27338587] [PMCID: 4918027] [DOI: 10.1186/s40168-016-0171-4]
[PMID: 29497420] [PMCID: 5818468] [DOI: 10.3389/fimmu.2018.00229]
[PMID: 17605583] [DOI: 10.1037/0894-4105.21.4.507]
[PMID: 16847772] [DOI: 10.1682/jrrd.2004.09.0120]
[PMID: 11286668] [DOI: 10.1007/s11926-001-0007-4]
[PMID: 19558254] [DOI: 10.1592/phco.29.7.800]
[PMID: 14529997] [DOI: 10.1016/s0003-4975(03)00817-8]
[PMID: 27573827] [PMCID: 5027464] [DOI: 10.1073/pnas.1607571113]
[PMID: 21178474] [PMCID: 3073172] [DOI: 10.4161/viru.1.5.12486]
[PMID: 20827765] [DOI: 10.1002/jmv.21873]
[PMID: 21543496] [PMCID: 3126563] [DOI: 10.1128/JVI.00693-11]
[PMID: 21383843] [PMCID: 3044169] [DOI: 10.1371/journal.pone.0017287]
[PMID: 19815723] [DOI: 10.1126/science.1179052]
[PMID: 21646307] [DOI: 10.1136/bmj.d3505]
[PMID: 17007934] [DOI: 10.1016/j.jad.2006.08.021]
[PMID: 17872383] [DOI: 10.1136/jcp.2007.050054]
[PMID: 12423773] [DOI: 10.1111/j.1574-695X.2002.tb00626.x]
[PMID: 11747919] [DOI: 10.1016/S0140-6736(01)06961-6]
[PMID: 16950834] [PMCID: 1569956] [DOI: 10.1136/bmj.38933.585764.AE]
[PMID: 335422]
[PMID: 11448704] [DOI: 10.1016/s0022-3999(01)00223-9]
[PMID: 10375340] [DOI: 10.7326/0003-4819-130-11-199906010-00016]
[PMID: 19855350]
[PMID: 11462315] [PMCID: 1314047]
[PMID: 16443043] [DOI: 10.1016/S0140-6736(06)68073-2]
[PMID: 20695975] [DOI: 10.1111/j.1365-2796.2010.02240.x]
[PMID: 11064960] [DOI: 10.1097/00004703-200010000-00003]
[PMID: 11200964] [DOI: 10.1017/s0033291799003001]
[PMID: 11595245] [DOI: 10.1016/s0022-3999(01)00247-1]
[PMID: 7490698] [DOI: 10.1016/0022-3999(95)00008-9]
[PMID: 15617866] [DOI: 10.1016/j.mehy.2004.07.037]
[PMID: 1281928] [DOI: 10.1126/science.1281928]
[PMID: 14525937] [DOI: 10.1096/fj.03-0396fje]
[PMID: 17822818] [DOI: 10.1016/j.cpr.2007.07.002]
[PMID: 17350740] [DOI: 10.1016/j.cpr.2007.01.010]
[PMID: 17021301] [PMCID: 1592057] [DOI: 10.1258/jrsm.99.10.506]
[PMID: 22039471] [PMCID: 3198463] [DOI: 10.1371/journal.pone.0026358]
[PMID: 30204780] [PMCID: 6133361] [DOI: 10.1371/journal.pone.0203503]