Main article: Pain medication and muscle relaxants

Table of Contents
Pain
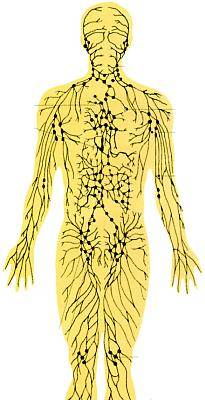
Pain is a common symptom in chronic inflammatory diseases. About 30% of the population of the United States suffers from acute or chronic pain, often of unknown cause.1) Any part of the body may be affected by inflammationThe complex biological response of vascular tissues to harmful stimuli such as pathogens or damaged cells. It is a protective attempt by the organism to remove the injurious stimuli as well as initiate the healing process for the tissue. resulting in pain. Lymph nodes are located all over the body and are prime suspects to swell and produce pain from immunopathologyA temporary increase in disease symptoms experienced by Marshall Protocol patients that results from the release of cytokines and endotoxins as disease-causing bacteria are killed. in chronic inflammatory diseases.
When pain has been chronic and severe, it is not unusual for inflammatory symptoms to be indicative of both longstanding and ongoing inflammation and immunopathology. For purposes of pain control, it is not necessary to differentiate. Adjusting the Marshall ProtocolA curative medical treatment for chronic inflammatory disease. Based on the Marshall Pathogenesis. (MP) medications is the best way to manage immunopathology including pain. If a patient's intolerable pain is not managed by adjustment of the MP medications, he or she should work with their doctor to use palliative methods for relief.
CytokinesAny of various protein molecules secreted by cells of the immune system that serve to regulate the immune system., Inflammation and Pain 2)
Management of pain
Inadequate pain control can impair the healing process. If patients' clinical picture is complicated and their pain severe, they might be best helped by consulting an expert in pain management at a local pain clinic.
Pain medications
Studies have shown that people in hospitals given adequate pain control tend to heal faster and are able to be discharged sooner than those who are not given adequate pain medications.3) The physiologic consequences of uncontrolled pain are myriad, and should not be overlooked.
For many patients, the level of pain is truly incapacitating and these patients have to have pain control just to be able to get through the day.4) The “tough it out” mentality can backfire for times when the pain simply becomes too much. For these patients, choosing to use pain medication is the realistic and inevitable choice.
As one proceeds on the MP, one will eventually get to the point where the pain medications can be weaned down and then off.
WARNING
Opioid-induced hyperalgesia (aka Paradoxical hyperalgesia), an extreme reaction to pain, is a phenomenon associated with the long-term use of opioids such as morphine, oxycodone, and methadone. OIH is characterized as generalized pain that is not necessarily confined to the affected site.
Over time, individuals taking opioids can develop an increasing sensitivity to noxious stimuli, even evolving a painful response to previously non-noxious stimuli (allodynia).
Tolerance, another condition that can arise from prolonged exposure to opioids, can often be mistaken for opioid-induced hyperalgesia and vice versa, as the clinical presentation can appear similar.
Massage and other manipulation therapies
Related article: Massage and other manipulation therapies
Related article: Pain
Massage, chiropractic, manual lymphatic drainage, and other manipulation therapies have been touted to alleviate symptoms of chronic disease. Those patients who are sicker or in an earlier stages of the Marshall Protocol (MP) have found that deep tissue massage can generate intolerable symptoms. These patients may want to avoid massage or any other therapies which cause a certain amount of tissue damage. Patients who want to try massage should start slowly and do only what feels beneficial and tolerable.
According to some patients, other more gentle manipulation therapies like craniosacral therapy or manual lymphatic drainage appear to improve symptoms.
For most conditions treated with a manipulation therapy, reviewers have concluded a lack of effectiveness or lack of well-conducted clinical trials.
Other strategies
Other strategies for managing pain include:
- managing anxiety and stress
- range of motion exercises – provided by University of Washington Orthopaedics and Sports Medicine; contains videos for movements exercises covering a range of body parts
- water exercises – provided by University of Washington Orthopaedics and Sports Medicine; contains videos for movements exercises covering a range of body parts
- TENS (Transcutaneous Electrical Nerve Stimulation) – battery-powered unit which sends electrical impulses through electrodes placed on or near the painful site
- elective surgery – MP patients are advised to postpone elective surgery as long as possible. Many MP patients discover they no longer need surgery once the inflammation is resolved.
- visualization techniques
- marijuana – Marijuana has been used by some patients with chronic pain such as ALS.5) Legality of use varies widely by jurisdiction. Please follow all relevant laws.
- physical activity and exercise – may increase tissue perfusion
- adequate rest – fatigue always worsens pain
- soak in a warm bath – use Epsom salts
- memory foam pad – for bed or chair; can relieve joint and back pain
Specific types of pain
Immunopathology can aggravate pain in areas of infection. Immunopathology can increase this inflammation and the resulting pain. This pain may be relieved by adjusting MP medications or taking pain medications.
Abdominal pain
Get medical attention anytime you have constant, unexplained abdominal pain, particularly if you also have fever and constipation or diarrhea.
Back pain
Some patients note the “pain of lying down,” and other back pain. Greg Blaney, MD has found that a lot of idiopathic (of unknown cause) spinal pain patients respond to the MP, and many actually exhibit overt Th1 metabolites
In my opinion, there is a definite correlation between disc disease and Th1. It being at the C7-T1 area (C8 is the nerve, not the vertebra) could also indicate a problem with the upper rib cage. C7 is where most of the neck extension occurs and that disc could be more vulnerable to mechanical stress if there is a upper rib restriction.
Restricted upper rib motion can be diagnosed by a number of means. One, palpation by therapist trained in osteopathy. Two, reduction or absense of radial (wrist) pulse with elevation of arm to horizontal, 1st rib; or above head 3rd rib. Treatment is to re-establish normal movement usually using manual techniques.
Both pathological calcification caused by vitamin D dysregulation and inflammation of the dorsal roots of the spinal nerves are seen in Th1 diseasesThe chronic inflammatory diseases caused by bacterial pathogens. and improve with the MP. However, improvement is usually later in phase 2 or 3 and can be associated with increased symptoms earlier.
Also, the cytokines found in tick borne diseases which are one source of Th1 pathogensThe community of bacterial pathogens which cause chronic inflammatory disease - one which almost certainly includes multiple species and bacterial forms., have been shown to weaken connective tissue and can cause a variety of hernias including disc herniation.
Greg Blaney, MD
Coccyx pain
A special cushion called a tush cush can be used to control coccyx immunopathology.
Immunopathology can result in increased inflammation in the back, which can be painful. It may be affecting either nerves or muscles, but immunopathology is temporary. It gives you a good idea of where all the problems are.
The best advice as per keeping the immune system reactions tolerable. It's easier to control it than to try to regain control.
Headache and migraines
Main article: Headaches and migraines
Different researchers have successfully used ARBs – of which olmesartan (Benicar)Medication taken regularly by patients on the Marshall Protocol for its ability to activate the Vitamin D Receptor. is one – to treat migraines and headaches.6)7) For patients on the Marshall Protocol (MP), the institution of the olmesartan (Benicar) blockade is enough to resolve migraines.
Flank pain
Related article: Kidney stones
Flank pain has a variety of causes. It can indicate immunopathology or a structural kidney problem such as kidney stones or simply muscle spasm.
The kidneys are in the back, one on each side of the spine. They are about 2 inches (5 cm) deep, just behind the lower ribs. Pain in a kidney is usually felt as upper back pain, on one side or the other. The pain can run down into the groin, or further down the back. The kidneys lie next to the muscles of the back, so that it can sometimes be difficult to tell the difference between muscle pain, back pain or kidney pain.
There are many causes of kidney pain. Infection in the kidney and kidney stones are the two common causes. X-ray tests will detect kidney stones. Samples of urine will be sent to the laboratory for culture tests to see if infection is present. Other conditions which cause some swelling or irritation of the kidneys may also cause pain, and these often fall into the category of “loin pain-haematuria syndrome.”
Detailed medical history questions might help determine if a patient's pain is related to one's kidneys.
Shoulder pain
Shoulder pain may occur with or without relation to current or previous injury and is often due to Th1 inflammationThe complex biological response of vascular tissues to harmful stimuli such as pathogens or damaged cells. It is a protective attempt by the organism to remove the injurious stimuli as well as initiate the healing process for the tissue. in the area. Shoulder pain may radiate down the arm with movement.
Limiting arm and shoulder movement to decrease pain may result in a “frozen shoulder” which can be very difficult to reverse. Frozen shoulder can be prevented by doing gentle range of motion exercises at home. If shoulder movement is already limited, it may be resolved by a combination of the Marshall Protocol, range of motion therapy and physical therapy. If surgery is suggested, these measures should be tried first.
MP patients are advised not to go under anesthesia to have any adhesions manipulated. Though noninvasive such a procedure will have a profound impact on the tissues in a patient's joint and one cannot be guaranteed the outcome will be positive.
Dental pain
The 'old wives' remedy is clove oil, a drop applied at site of pain by means of a cotton bud.
related article working with a dentist
Patient interviews

neurosarcoidosis, systemic sarcoidosis; spasticity, myasthenia, CNS dysfunction, joint pain, pulmonary, splenic and cardiac involvement
Read the interview
Patients experiences
This was not unexpected, but I thought I'd share in case someone looks up plantar fasciitis on the MP. Within in months of becoming nearly totally bed bound in November 2003, I had a severe case of plantar faciitis (which the foot doctor told me was impossible to have as a result of being bed bound), and I would have to wear shoes with molded foot beds in them just to cross the ten feet between my bed and the toilet. After two years on the MP (fall 2008), I was once again able to walk around bare foot on my hardware floors.
eClaire, MP-Lifestyles.org
Earlier this week Opa visited his doctor and asked for buprenorphine. He had brought a printout of the pain physician article with him. Doc prescribed him the sublingual form.
Opa already confirmed that the new pain medication helps to contol his acute pain during IP surges.
Ron, MarshallProtocol.com
My lifelong back pain dropped significantly. This is a strange new world I live in with very little back pain. Who could have imagined it had anything to do with an infection.
Davbkr, MarshallProtocol.com
I have had decades of chronic back issues with years of various interventions: manipulation, ultrasound, physical therapy, water therapy, massage, exercise, acupuncture, etc. Thankfully, I've now recovered from all forms of stiffness, pain, and spasms, so the MP did resolve the inflammation that was obviously the unrelenting culprit.
However, whether it were then or now, prolonged bed rest and back pain go hand-in-hand. A sustained position of any sort, for me, would always aggravate my back. Even after back surgery twenty-six years ago, the surgeon insisted that his patients get out of bed ASAP and “move.” I did take a muscle relaxer to be able to freely move and used a pain pill for only a brief period of time. We were encouraged to walk, walk, walk. Following that advice, I was able to leave the hospital before everyone else and was able to return to work the quickest.
One therapy, years later, that felt wonderful was in a heated pool with a physical therapist at a rehab center. My muscles responded very quickly to that treatment, and being able to exercise and see the progress gave me an emotional boost.
Carole, MarshallProtocol.com
[PMID: 21900506] [PMCID: 3250243] [DOI: 10.1096/fj.11-192898]
[PMID: 17426506] [PMCID: 2785020] [DOI: 10.1097/AIA.0b013e318034194e]
[PMID: 17667496] [PMCID: 1933564] [DOI: 10.1097/SLA.0b013e31805dac11]
[PMID: 17578977] [DOI: 10.1213/01.ane.0000268145.52345.55]
[PMID: 11467101] [DOI: 10.1177/104990910101800411]
[PMID: 12681087]
[PMID: 12503978] [DOI: 10.1001/jama.289.1.65]