
Table of Contents
Test: C-Reactive Protein (CRP)
C-reactive protein (CRP) is an important and evolutionarily ancient component of the innate immune responseThe body's first line of defense against intracellular and other pathogens. According to the Marshall Pathogenesis the innate immune system becomes disabled as patients develop chronic disease..1) CRP has been described as “the prototypical acute-phase reactant to infections and inflammationThe complex biological response of vascular tissues to harmful stimuli such as pathogens or damaged cells. It is a protective attempt by the organism to remove the injurious stimuli as well as initiate the healing process for the tissue. in human beings.” In the clinical setting, CRP is used “as a clinical indicator of acute infections and response to treatment, and to assess inflammatory status in chronic diseases.”2) Initially it was thought that CRP might be a pathogenic secretion as it was elevated in people with a variety of illnesses including cancer.3) However, discovery of synthesis in the liver demonstrated that it is manufactured by the human body.
The fact that CRP is an independent predictor of stroke and coronary artery disease but also a key contributor to effective bacterial clearance,4) underscores the importance of microbes in the pathogenesis of these diseases. Some patients on the Marshall ProtocolA curative medical treatment for chronic inflammatory disease. Based on the Marshall Pathogenesis. (MP) have reported temporary increases in CRP, an observation which is consistent with a heightened immune response.
CRP's name comes from its capacity to bind the C-polysaccharide of Streptococcus pneumoniae, which provides innate defense against pneumococcal infection.5)
Interpreting high CRP
An elevated CRP is something that is expected to be seen in many MP patients because it's a direct indicator of an inflammatory response to infection. The experience of Autoimmunity Research FoundationNon-profit foundation dedicated to exploring a pathogenesis and therapy for chronic disease. has, thus far, shows that as long as immunopathologyA temporary increase in disease symptoms experienced by Marshall Protocol patients that results from the release of cytokines and endotoxins as disease-causing bacteria are killed. is tolerable while CRP remains high, there's no need to make any changes in dosing of the MP medications. However, physicians and patients should always assess if immunopathology is too strong. If this is the case, taking measures to reduce immunopathology is always recommended. Patients with cardiac disease may want to be particularly careful about assessing the level of immunopathology when their CRP goes out of range.
Function
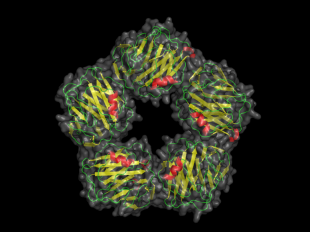
C-reactive protein is an acute phase reactant (that is, a substance rapidly produced after infection or tissue damage) with roles including:
- innate host defense – promotes phagocytosis by opsonizing bacteria (i.e. coating the microbe with antibodies or a complement protein so as to make it palatable to phagocytes)
- clearance of damaged cells – binds phosphocholine expressed on the surface of dead or dying (i.e. apoptotic, necrotic) human and bacterial cells
- regulation of the inflammatory response – may act through Fcgamma receptors to reduce inflammation and protect from certain autoimmune diseases6)
During the acute phase response, levels of CRP rapidly increase up to 1000-fold, reaching a peak at 48 hours. With resolution of the acute phase response, CRP declines with a relatively short half-life of 18 hours.7)
Demonstrated antimicrobial activity against gram-negative bacteria
CRP has been shown to be generated in response to several gram-negative species of bacteria including:
- Chlamydia pneumoniae – Johnson et al. showed that the presence of viable C. pneumoniae in patients who underwent endarterectomy for carotid artery stenosis independently predicted C-reactive protein levels.8)
- Psuedomonas aeruginosa – Ng et al. used a horseshoe crab animal model to demonstrate that serum levels of CRP are upregulated by about 60-fold in 6-48 hours after infection with the gram-negative bacterial pathogen, P. aeruginosa.9)
Of course, one of the structural components of gram-negative bacteria are endotoxins, the bioavailability of which leads to the immunopathological reactionA temporary increase in disease symptoms experiences by Marshall Protocol patients that results from the release of cytokines and endotoxins as disease-causing bacteria are killed. as described by the Marshall PathogenesisA description for how chronic inflammatory diseases originate and develop..
Predictor of cardiovascular disease
C-reactive protein is a predictor of:
- risk of cardiovascular events in patients with coronary artery disease13)
- development of hypertension14)
The association between serum C-reactive protein levels and subsequent risk of stroke, heart attack, and death from cardiac causes supports the importance of inflammation and chronic infection in the pathogenesis of cerebrovascular and coronary artery disease.15) 16)
Because there are a large number of disparate conditions that can induce CRP production, an elevated CRP level does not have diagnostic specificity.17)
A more sensitive CRP test, called a highly sensitive C-reactive protein (hs-CRP) assay, is available to determine heart disease risk.
Other diseases
In addition to the blood serum, CRP has also been detected in the cerebrospinal fluid,18) which suggests the protein could be secreted in response to microbial infection.
CRP also tends to be associated with other chronic inflammatory diseases including rheumatoid arthritis, ankylosing spondylitis, Crohn's disease, and psoriatic arthritis. While elevated levels of CRP are an indication of ongoing infection and inflammation of many such diseases, it is certainly not present in all diseases. For example, conditions such as systemic lupus erythematosus, ulcerative colitis, and scleroderma tend to present with modest, if not absent, increases in CRP.19)
Ultimately, the absence of CRP as a sensitive marker for inflammatory disease may parallel the inconsistency with which any one species of pathogen is found in chronic disease. It would appear that the body employs a variety of mechanisms for responding to infection, only one of which is the production of CRP.
Read more
[PMID: 15198851] [DOI: 10.1179/096805104225004833]
[PMID: 19000576] [DOI: 10.1016/j.jaci.2008.10.002]
[PMID: 12813013] [PMCID: 161431] [DOI: 10.1172/JCI18921]
[PMID: 16176663] [DOI: 10.1179/096805105X37402]
[PMID: 15531769] [DOI: 10.1385/IR:30:3:261]
[PMID: 11739967] [DOI: 10.1161/hs1201.099631]
[PMID: 8797513] [DOI: 10.1093/oxfordjournals.aje.a008963]
[PMID: 9727541] [DOI: 10.1161/01.cir.98.8.731]
[PMID: 9077376] [DOI: 10.1056/NEJM199704033361401]
[PMID: 11036126] [DOI: 10.1056/NEJM200010193431609]
[PMID: 14665655] [DOI: 10.1001/jama.290.22.2945]
[PMID: 9887164] [DOI: 10.1056/NEJM199901143400207]
[PMID: 16818927] [DOI: 10.7326/0003-4819-145-1-200607040-00129]
[PMID: 11861461]

