Related article: Skin conditions

Table of Contents
Psoriasis
Psoriasis is an autoimmune disease that affects the skin that varies in severity from minor localized patches to complete body coverage. The richness of the skin microbiome and the emerging discrepancies between the microbial composition between health and disease point to a microbial etiology for psoriasis.
The Marshall ProtocolA curative medical treatment for chronic inflammatory disease. Based on the Marshall Pathogenesis. treats psoriasis by reactivating the innate immune responseThe body's first line of defense against intracellular and other pathogens. According to the Marshall Pathogenesis the innate immune system becomes disabled as patients develop chronic disease.. In the course of treatment, patients' disease symptoms may become worse due to a process called immunopathologyA temporary increase in disease symptoms experienced by Marshall Protocol patients that results from the release of cytokines and endotoxins as disease-causing bacteria are killed..
Skin microbiome
A decade ago, Chiller et al. concluded, “The skin is a poor media for bacteria given the large number of inherent defense mechanisms.”1) This assessment was undermined seven years later by Fierer et al.’s work, which found that the average human palm harbors at least 150 bacterial species – an order of magnitude greater than previous estimates.2) A 2009 Science study expanded on this understanding of microbial diversity in skin, showing that forearms and underarms, though located just a short distance apart, are as “ecologically dissimilar as rainforests are to deserts.”3) Trillions of bacteria, fungi, viruses, archaea, and small arthropods colonize the skin surface, collectively comprising the skin microbiome.4) One prominent researcher called human skin a “virtual zoo of bacteria.”5)
Novel insights are being revealed about the extent to which skin microbiotaThe bacterial community which causes chronic diseases - one which almost certainly includes multiple species and bacterial forms. affects health. For example, odors produced by skin microbiota are attractive to mosquitoes as shown by in vitroA technique of performing a given procedure in a controlled environment outside of a living organism - usually a laboratory. studies, and variation in bacterial species on the human skin may explain the variation in mosquito attraction between humans.6)
Evidence of infectious cause
- cell wall deficient bacteria – In a 2009 study, Wang investigated the carriage rate of cell wall deficient bacteria in the tonsil or pharynx of psoriasis patients. Cell wall deficient bacteria, a term often used interchangeably with l-formDifficult-to-culture bacteria that lack a cell wall and are not detectable by traditional culturing processes. Sometimes referred to as cell wall deficient bacteria., were isolated from 74.2% of psoriasis patients, 23.5% of chronic tonsillitis patients and only 6.3% of controls.7)
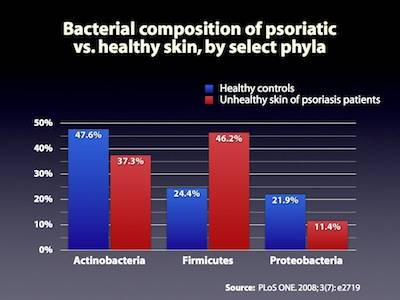
- differences in microbiotaThe bacterial community which causes chronic diseases - one which almost certainly includes multiple species and bacterial forms. between psoriasis and normal skin – A 2008 study of psoriatic skin not only found 84 novel species never before known to persist in skin, but also double the proportion of microbes from the Firmicutes phylum in psoriatic patients, as compared to healthy controls.8) In contrast, Fahlén's study analyzed 10 psoriatic patients using pyrosequencing,9) finding no difference in levels of Firmicutes but confirmed lower levels of Propionibacterium. The discrepancies between these two studies illustrate the importance of focusing on the activity of microbes and as well as the competence of the immune response.
- bacterial DNA in blood of psoriatic patients – Peripheral blood samples from 20 patients with psoriasis and from 16 control subjects were studied for the presence of bacteria by PCR using universal 16S ribosomal DNA primers and specific primers for S. pyogenes. Sequence analysis of amplified 16S rRNA sequences was used to determine taxonomic identity. Ribosomal bacterial DNA was detected in the blood of all 20 patients with psoriasis, but in none of the controls.10)
Other treatments
For many physicians, immunosuppressive medications are a first-line treatment for psoriasis. These drugs suppress the innate immune response, which provides some patients with temporary symptom palliation, because they reduce immunopathology, the bacterial die-off reaction.
- corticosteroidsA first-line treatment for a number of diseases. Corticosteroids work by slowing the innate immune response. This provides some patients with temporary symptom palliation but exacerbates the disease over the long-term by allowing chronic pathogens to proliferate. – For even short periods of time, steroid use can become genuinely addictive. Research shows that any kind of short-term symptomatic improvement from corticosteroidA first-line treatment for a number of diseases. Corticosteroids work by slowing the innate immune response. This provides some patients with temporary symptom palliation but exacerbates the disease over the long-term by allowing chronic pathogens to proliferate. use does not last, and that over the longer term, use of the drugs entales a litany of side effects. For their own safety, patients on the Marshall Protocol (MP) must wean off of them as opposed to discontinuing them outright.
- TNF-alphaA cytokine critical for effective immune surveillance and is required for proper proliferation and function of immune cells. inhibitors – Tumor necrosis factor-alphaA cytokine critical for effective immune surveillance and is required for proper proliferation and function of immune cells. or TNF-alpha is a cytokineAny of various protein molecules secreted by cells of the immune system that serve to regulate the immune system. critical for effective immune surveillance.11) TNF-alpha inhibitors, also known as TNF blockers, anti-TNF drugsDrugs which interfere with the body's production of TNF-alpha - a cytokine necessary for recovery from infection or TNF-alpha antagonists, are drugs which interfere with the body's production of TNF-alpha.12) Anti-TNF drugs are expensive, ineffective at treating chronic disease and have a number of adverse effects such as increase risk of serious infection such as mycobacterial infection.13) 14)
- methotrexate – Methotrexate (MTX) is an antibiotic that interferes with bacteria's ability to synthesize folate. It is used to treat diseases with rapid cell growth such as cancer and some autoimmune diseases, particularly the rheumatic diseases. A superior alternative to MTX is the Marshall Protocol antibiotic, Bactrim DS.
- light therapy – Phototherapy suppresses immunity which can lead to the progression of other infections such as human papilloma virus (HPV). A 2010 study used a nested polymerase chain reaction, to analyze skin biopsies taken a from 20 psoriasis patients under phototherapy (UVB) and 20 untreated psoriatic patients. The authors were able to detect viruses in 60% of the treatment but in none of the controls.15) In reality, light therapy does nothing to resolve underlying disease state and can actually delay progress for MP patients. Certainly prolonged light exposure has been shown to increase skin melanoma – the World Health Organization now categorizes tanning beds under the highest cancer risk category.16) MP patients who have completed the treatment have been able to attest to the fact that sunshine is not necessary for good health or happiness.
Research
Antimicrobial peptidesBody’s naturally produced broad-spectrum antibacterials which target pathogens. (AMPs) are strongly expressed in lesional skin in psoriasis and play an important role as proinflammatory “alarmins” in this chronic skin disease. Vitamin D analogs like calcipotriol have antipsoriatic effects and might mediate this effect by changing AMP expression. In this study, keratinocytes in lesional psoriatic plaques showed decreased expression of the AMPs beta-defensin An antimicrobial peptide found primarily in immune cells and transcribed by the Vitamin D Receptor. (HBD) 2 and HBD3 after topical treatment with calcipotriol. At the same time, calcipotriol normalized the proinflammatory cytokine milieu and decreased interleukin (IL)-17A, IL-17F and IL-8 transcript abundance in lesional psoriatic skin. In contrast, cathelicidin Family of antimicrobial peptides found primarily in immune cells and transcribed by the Vitamin D Receptor. antimicrobial peptide expression was increased by calcipotriol while psoriasin expression remained unchanged. In cultured human epidermal keratinocytes the effect of different vitamin D analogs on the expression of AMPs was further analyzed. All vitamin D analogs tested blocked IL-17A induced HBD2 expression by increasing IkappaB-alpha protein and inhibition of NF-kappaBA protein that stimulates the release of inflammatory cytokines in response to infection signaling. At the same time vitamin D analogs induced cathelicidin through activation of the vitamin D receptorA nuclear receptor located throughout the body that plays a key role in the innate immune response. and MEK/ERK signaling. These studies suggest that vitamin D analogs differentially alter AMP expression in lesional psoriatic skin and cultured keratinocytes. Balancing AMP “alarmin” expression might be a novel goal in treatment of chronic inflammatory skin diseases. 17)
Patients experiences
I've had lots of experience with psoriasis (which looks like sarc lesions, BTW). I've found a cream that helps it feel better. It's a combo of mango and shea butter that I buy at Walmart, made by Tree Hut. It's very soothing.
Reenie, MarshallProtocol.com
Patient interviews
[PMID: 11924823] [DOI: 10.1046/j.0022-202x.2001.00043.x]
[PMID: 19004758] [PMCID: 2584711] [DOI: 10.1073/pnas.0807920105]
[PMID: 19478181] [PMCID: 2805064] [DOI: 10.1126/science.1171700]
[PMID: 22189793] [PMCID: 3279608] [DOI: 10.1038/jid.2011.417]
[PMID: 17293459] [PMCID: 1815283] [DOI: 10.1073/pnas.0607077104]
[PMID: 20840217] [DOI: 10.1111/j.1574-6941.2010.00908.x]
[PMID: 20137493]
[PMID: 18648509] [PMCID: 2447873] [DOI: 10.1371/journal.pone.0002719]
[PMID: 22065152] [DOI: 10.1007/s00403-011-1189-x]
[PMID: 20607546] [DOI: 10.1007/s00403-010-1065-0]
[PMID: 16331857] [DOI: 10.1007/3-540-37673-9_10]
[PMID: 16705109] [DOI: 10.1001/jama.295.19.2275]
[PMID: 12614731] [DOI: 10.1016/s1473-3099(03)00545-0]
[PMID: 20415738] [DOI: 10.1111/j.1600-0781.2010.00492.x]
[PMID: 19655431] [DOI: 10.1016/s1470-2045(09)70213-x]
[PMID: 19623255] [PMCID: 2709447] [DOI: 10.1371/journal.pone.0006340]