Related articles: Crohn's disease and ulcerative colitis, Celiac disease

Table of Contents
Irritable bowel syndrome (IBS)
Irritable bowel syndrome (IBS) is a gastrointestinal disorder characterized by chronic abdominal pain and altered bowel habits. It is the most commonly diagnosed gastrointestinal condition: the prevalence of IBS in North America is estimated to be approximately 10 to 15 percent Until the advent of culture-independent studies, physicians supposed IBS was a psychosomatic (functional) disorder as there was limited indication of an organic cause, with physicians complaining that patients were unmotivated to seek out cognitive behavioral therapy.1)
However, the notion that IBS is a psychological disorder has come under serious challenge.2) Recent research demonstrates that IBS is characterized by significant alterations in the gut microbiotaThe bacterial community which causes chronic diseases - one which almost certainly includes multiple species and bacterial forms..3)
The Marshall ProtocolA curative medical treatment for chronic inflammatory disease. Based on the Marshall Pathogenesis. treats IBS by reactivating the innate immune responseThe body's first line of defense against intracellular and other pathogens. According to the Marshall Pathogenesis the innate immune system becomes disabled as patients develop chronic disease.. In the course of treatment, patients' disease symptoms may become worse due to a process called immunopathologyA temporary increase in disease symptoms experienced by Marshall Protocol patients that results from the release of cytokines and endotoxins as disease-causing bacteria are killed..
Symptoms
As a matter of course, symptoms of IBS will fluctuate while a patient is on the Marshall Protocol (MP). In addition to the strategies outline in the Managing immunopathology article, the following may also be helpful:
- constipation – MP patients with constipation should have the symptom treated for immediate relief and then measures should be adopted to prevent constipation.
- diarrhea – Patients with diarrhea may wish to increase fluid intake and/or take anti-diarrheal medication. 4)
- loss of appetite – If nausea is preventing a patient from eating, it's very important to palliate the nausea. Over the counter medications such as Gravol (dramamine) may be helpful. If not, patients should ask their doctor for a prescription antiemetic, such as hydroxyzine.
Evidence of infectious cause
Recent studies provide increasing support for the concept that disturbances in gut flora occur in patients with irritable bowel syndrome and that such abnormalities may contribute to irritable bowel syndrome-type symptoms.
Riordan et al.5)
Onset following gastrointestinal infection
Epidemiologic studies have shown that gastrointestinal infection is the strongest environmental risk factor for the development of IBS.6) 7) Although most patients with gastroenteritis become asymptomatic, a small but significant proportion of subjects (7%–31%) develop postinfectious IBS, dyspepsia, or both. A recent systematic review and meta-analysis identified that the incidence for IBS development after infectious gastroenteritis was 10%.8)
Abnormal composition
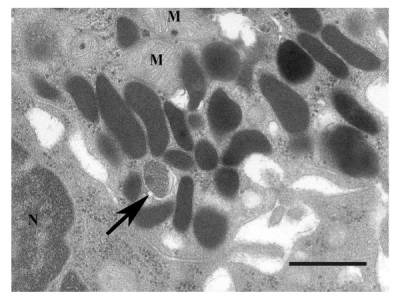
Small intestinal bacterial overgrowth (SIBO) has been documented in a proportion of patients with IBS (10%–84%). For example, in 2012, Greek researchers enrolled patients needing upper gastrointestinal (GI) tract endoscopy. Among 320 subjects SIBO was diagnosed in 62 (19.4%) with 42 of those having IBS (67.7%). Of all IBS sufferers, SIBO was found in 37.5%. Escherichia coli, Enterococcus spp. and Klebsiella pneumoniae were the most common isolates within patients with SIBO. Several researchers have shown that eradicating SIBO results in symptomatic improvement.9) 10)
Higher temporal instability
Accumulating evidence shows that patients with IBS have a higher temporal instability of the bacterial populations and that the microbiota composition is different compared with healthy controls.11) 12)
Headline
Free versus total serum 25-hydroxyvitamin D in a murine modelA model of disease which uses rats or mice to mimic human conditions. of colitis. 13)
Further research
Findings suggest that neither olmesartanMedication taken regularly by patients on the Marshall Protocol for its ability to activate the Vitamin D Receptor. Also known by the trade name Benicar. nor other ARBs were associated with diarrhea among patients undergoing endoscopy. The spruelike enteropathy recently associated with olmesartan is likely a rare adverse effect and milder presentations are unlikely. 14)
In a methotrexate-induced model of intestinal mucositis, olmesartan reduced inflammationThe complex biological response of vascular tissues to harmful stimuli such as pathogens or damaged cells. It is a protective attempt by the organism to remove the injurious stimuli as well as initiate the healing process for the tissue. and induced enteropathy characterized by severe diarrhea, weight loss, and reduced sucrose activity. 15)
Mast cell activation syndromes 16)
Gastrointestinal (GI) symptoms are commonly reported in patients with mast cell disease. 17)
Mast cells are located in close proximity to the vasculature, and vasoactive mediators released upon their activation can promote endothelial activation leading to blood brain barrier (BBB) dysfunction. 18)
Mast cell activation plays an important role in stress-mediated disease pathogenesis. 19)
Patient interviews

Lyme disease, irritable bowel syndrome/ulcerative colitis, radiculitis
Read the interview

Interviews of patients with other diseases are also available.
[PMID: 20484720] [DOI: 10.1176/appi.psy.51.3.225]
[PMID: 17040359] [PMCID: 1761148] [DOI: 10.1111/j.1445-5994.2006.01217.x]
[PMID: 20937460] [DOI: 10.1016/j.idc.2010.07.005]
[PMID: 26203094] [PMCID: 4548161] [DOI: 10.3945/jn.115.212308]
[PMID: 17053447] [DOI: 10.1097/01.mog.0000245544.80160.46]
[PMID: 10037630] [PMCID: 27756] [DOI: 10.1136/bmj.318.7183.565]
[PMID: 17445753] [DOI: 10.1016/j.cgh.2007.02.008]
[PMID: 17661757] [DOI: 10.1111/j.1365-2036.2007.03399.x]
[PMID: 11151884] [DOI: 10.1111/j.1572-0241.2000.03368.x]
[PMID: 12591062] [DOI: 10.1111/j.1572-0241.2003.07234.x]
[PMID: 15747442] [DOI: 10.1016/j.femsim.2004.08.009]
[PMID: 19693670] [DOI: 10.1007/s10620-009-0934-x]
[PMID: 25023670] [PMCID: 4157109] [DOI: 10.1016/j.mayocp.2014.05.012]
[PMID: 25947920] [DOI: 10.1248/bpb.b14-00847]
[PMID: 30837843] [PMCID: 6389675] [DOI: 10.3389/fncel.2019.00054]

