Main article: Successive infection and variability in disease

Table of Contents
Asthma
Asthma has been conventionally understood to be a misdirected immune reaction to environmental exposures, but this explanation is being challenged by recent metagenomic studies. Culture-independent studies have shown, consistent with successive infectionAn infectious cascade of pathogens in which initial infectious agents slow the immune response and make it easier for subsequent infections to proliferate., that early infections predispose to asthma. Work also suggests that the lung microbiome is different in asthmatic patients compared to healthy controls.
Papadopoulos et al. have written that asthma should be treated as a suboptimal innate immune responseThe body's first line of defense against intracellular and other pathogens. According to the Marshall Pathogenesis the innate immune system becomes disabled as patients develop chronic disease..1) Consistent with that thinking, the Marshall ProtocolA curative medical treatment for chronic inflammatory disease. Based on the Marshall Pathogenesis. (MP) is a treatment for asthma. While many physicians still consider immunosuppressive medications such as corticosteroidsA first-line treatment for a number of diseases. Corticosteroids work by slowing the innate immune response. This provides some patients with temporary symptom palliation but exacerbates the disease over the long-term by allowing chronic pathogens to proliferate. as a first-line treatment for asthma, these drugs interfere with the body's immune response. The Marshall Protocol is designed to stimulate the innate immune response. In the process may cause immunopathologyA temporary increase in disease symptoms experienced by Marshall Protocol patients that results from the release of cytokines and endotoxins as disease-causing bacteria are killed., the bacterial die-off reaction.
Lung microbiome
Until recently, estimates of the resident microbial flora in the lungs were far too low. A 1998 infectious disease textbook stated that the lungs were sterile.2) However, such conclusions were made on the basis of culture-based tests, which we now know identify a small minority of microbes. Since then, metagenomic analyses have indicated the presence of a persistent lung microbiome, the composition of which differs in health and disease. For example, Erb-Downward found bacterial 16S sequences in the lung tissues of all subjects in a 2011 based study of healthy patients as well as those with chronic obstructive pulmonary disease (COPD).3)
Evidence of infectious cause
Asthma has been conventionally understood to be a misdirected immune reaction to environmental exposures, but this explanation is being challenged.
People thought that asthma was caused by inhalation of allergens but this study shows that it may be more complicated than that – asthma may involve colonization of the airways by multiple bacteria.
Homer Boushey, MD, UCSF professor of medicine
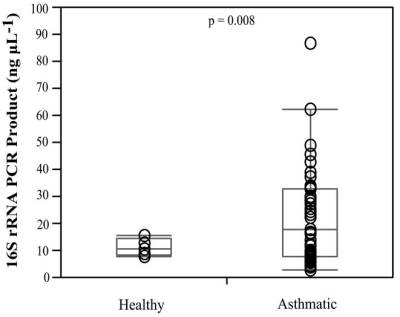
In their three-year pilot project, Huang et al. collected samples from the airway linings of 65 adults with mild to moderate asthma and 10 healthy subjects.4) Then, using 16S rRNA – a tool that can identify approximately 8,500 distinct groups of bacteria in a single assay – the scientists profiled the organisms present in each sample to look for relationships between bacterial community composition and clinical characteristics of the patients' asthma.
Airway microbiotaThe bacterial community which causes chronic diseases - one which almost certainly includes multiple species and bacterial forms. composition and diversity were significantly correlated with bronchial hyperresponsiveness. Specifically, the relative abundance of particular phylotypes, including members of the Comamonadaceae, Sphingomonadaceae, Oxalobacteraceae and other bacterial families, were highly correlated with the degree of bronchial hyperresponsiveness.
Successive infection
There is broad support for the conclusion that early infections, especially acute infections, predispose a person to later onset of chronic diseases such as asthma. Successive infection is the process by which an infectious cascade of pathogens slow the immune response and allow for subsequent infections (and the diseases which they cause) to proliferate. For example:
- rhinoviruses in infancy – Children who experience repeated rhinovirus-induced wheezing episodes in infancy have a significantly increased risk of developing asthma.5)
- neonates and common infections – Neonates colonized in the hypopharyngeal region with S. pneumoniae, H. influenzae, or M. catarrhalis, or with a combination of these organisms, are at increased risk for recurrent wheeze and asthma early in life.6)
Management and treatment
Related article: Managing immunopathology
Papadopoulos et al. have written that asthma should be treated as a suboptimal innate immune response.7) Consistent with that thinking, the Marshall Protocol is a treatment for asthma. Other treatments (some of which are contraindicated) include the following.
Immunosuppressive medications
For many physicians, immunosuppressive medications are a first-line treatment for asthma. These drugs suppress the innate immune response, which provides some patients with temporary symptom palliation, because they reduce immunopathology, the bacterial die-off reaction.
- corticosteroids – There are no studies which show that glucocoritcoids (corticosteroids) improve long-term prognosis in the treatment of illness. Van den Bosch and Grutters write8), “Remarkably, despite over 50 years of use, there is no proof of long-term (survival) benefit from corticosteroidA first-line treatment for a number of diseases. Corticosteroids work by slowing the innate immune response. This provides some patients with temporary symptom palliation but exacerbates the disease over the long-term by allowing chronic pathogens to proliferate. treatment.” For even short periods of time, steroid use can become genuinely addictive. Research shows that any kind of short-term symptomatic improvement from corticosteroid use does not last, and that over the longer term, use of the drugs entales a litany of side effects. For their own safety, patients on the MP must wean off them as opposed to discontinuing them outright.
- inhalers, steroid – Steroid inhalers suppress the innate immune response and delay progress on the MP. MP patients taking steroid inhalers should work with their physicians to switch drugs such as a bronchiodilator inhaler.
Vitamin D
Several studies have shown that patients with asthma have low levels of the vitamin D metabolite, 25-DThe vitamin D metabolite widely (and erroneously) considered best indicator of vitamin D "deficiency." Inactivates the Vitamin D Nuclear Receptor. Produced by hydroxylation of vitamin D3 in the liver..9) 10) While some in the medical community have been quick to conclude this suggests a need for supplementation, supplemental vitamin D interferes with the immune response precisely when it needs to respond to microbes and may therefore contribute to asthma.
Hansen et al. study with 965 pregnant women enrolled in 1988-1989 does not provide support for a protective effect of a high maternal 25(OH)D concentration on outcomes of allergic airway disease and lung function at 20 to 25 years of age. In contrast, a high maternal 25(OH)D concentration might be associated with an increased risk of allergic diseases in offspring. 11)
Hyppönen et al. performed a retrospective cohort study of 7,648 Finnish infants born in 1967. The prevalence of asthma at age 31 years was 35% higher in participants who had received vitamin D supplementation regularly during the first year compared to others.12) A stronger relationship between cod liver oil supplementation (which is high in vitamin D) and asthma was likewise identified in an Australian study.13)
Other treatments
- inhalers, bronchiodilator – A bronchodilator is a substance that dilates the bronchi and bronchioles, decreasing airway resistance and thereby facilitating airflow. A bronchodilator is delivered either by Medicated Dose Inhalers (MDI) or Dry Powder Inhalers (DPI) may be useful to reduce shortness of breath (dyspnea). As opposed to steroid inhalers, which are immunosuppressive, it is okay and sometimes essential to use bronchodilators while on the MP. Note that some combination products including Seretide, Advair, and Symbicort contain both bronchiodilating and steroidal medications and are therefore contraindicated.
- supplemental oxygen – Some patients with obstructive lung diseases have trouble getting enough oxygen by breathing normally. For these patients, a prescription for supplemental oxygen should be seriously considered. Supplemental oxygen may be useful or necessary in some cases even though it may be needed only for a few hours a day for a few months. Some patients may need oxygen when flying or at high altitude.
- air purifier – Methotrexate (MTX) and sulfasalazine are antimetabolite antibiotics with actions similar to Bactrim DS, an MP antibiotic. MP patients taking MTX or sulfasalazine must discontinue those medications.
- breathing exercises – acceptable, as time allows; may reduce anxiety, oxygenate tissues
Epidemiology
Asthma is one of the most common diseases in the world, with approximately 300 million asthmatics globally, including 24 million in the United States, according to the Centers for Disease Control. The disease has been on the rise for the last 60 years. “It has gone from 3 percent of the population to slightly more than 8 percent of the population in the U.S.,” according to Homer Boushey.
Patients experiences
I can tell you from personal experience that I too had to get off my steroid inhaler when I started the MP. I was so scared to do this, as my asthma was so bad. Much to my relief, the Benicar was better than the steroid inhaler! I also used a long acting (12-hour) non-steroidal inhaler, but after one year on the MP, I no longer needed it. I do still use the short-acting inhaler four times a day, but only need one puff.
My asthma is triggered by MCS. The MCS has also improved on the MP. I actually once left the house without my inhaler, and the Benicar stopped my asthma attack within 10 minutes. I should have chewed and put it under my tongue, but I was not thinking. This allows for quicker absorption. I was so impressed that the Benicar could do this.
Lori, MarshallProtocol.com
I had Chronic Lyme undiagnosed when I started to work in a building with a brook in the back. This brook would overflow upon heavy rain, causing a SEVERE mold issue for me. (worked there for 2 years) I never had asthma till then. I collapsed at work, 7 years ago. It took me another year to finally get my Lyme diagnosis. I was on a nebulizer, steroid inhaler, bronchial inhaler, rescue inhaler and oral medication for my lungs. All at the same time. (nebulizer for 1 year) I was a mess.
After finally getting the Lyme diagnosis, I was put on 1,000mg of Ceftin and 500mg of Zithromax a day for 4 years. Also had 1 month of IV treatment, 1 year apart. Then put on Minocycline 100mg. This DID NOT help. I also wore a personal air purfier around my neck for 5 years 24/7, due to MCS, which exacerbated my Asthma.
I have been on the MP for 22 months. I had to get off the steroid inhaler in order to start the MP. I was scared to do this, but the Benicar seemed to help a great deal with the inflammationThe complex biological response of vascular tissues to harmful stimuli such as pathogens or damaged cells. It is a protective attempt by the organism to remove the injurious stimuli as well as initiate the healing process for the tissue.. After 8 months, I was able to stop the meds I used to take for all my other conditions. After 12 months, I no longer could take the 12 hour ( long acting) bronchial inhaler. It would make me feel ill. I am only using my rescue inhaler 4 times a day, to control my Asthma. My MCS has improved, thus not being such a big trigger anymore. Benicar actually stopped an Asthma attack I was having when out, within 10 minutes. (I should have chewed and put it under my tongue) I had left my inhaler home, and felt doomed, then tried the Benicar, and WOW.
After 16 months on the MP, I no longer wear the air purfier!!!!! The adjustable bed I have, I used to sleep at an 85 degree angle (almost totally upright), now I can sleep at a 45 degree angle with a pillow (I was not able to take the pressure of a pillow on my back before the MP).
I am on low doses of phase 3 abx on the MP, and I am having wonderful results!!!!!
This should give you a good idea just HOW much the MP has helped my Asthma.
Take Care.
Lori, MarshallProtocol.com
[PMID: 17188832] [PMCID: 7135156] [DOI: 10.1016/j.biopha.2006.10.004]
[PMID: 21364979] [PMCID: 3043049] [DOI: 10.1371/journal.pone.0016384]
[PMID: 21194740] [PMCID: 3037020] [DOI: 10.1016/j.jaci.2010.10.048]
[PMID: 22053589]
[PMID: 17928596] [DOI: 10.1056/NEJMoa052632]
[PMID: 16946094] [DOI: 10.1183/09031936.06.00105805]
[PMID: 19179486] [PMCID: 2675563] [DOI: 10.1164/rccm.200808-1361OC]
[PMID: 19365260] [PMCID: 2897155] [DOI: 10.1097/ACI.0b013e32832b36cd]
[PMID: 25649083] [DOI: 10.1016/j.jaci.2014.12.1924]
[PMID: 15699498] [DOI: 10.1196/annals.1337.013]
[PMID: 20880353] [DOI: 10.1111/j.1399-3038.2010.01099.x]

