Table of Contents
Autism spectrum disorder
Autism is a disorder of neural development characterized by impaired social interaction and communication, and by restricted and repetitive behavior. These signs often begin before a child is three years old.
A study, led by Dr. Xiaosi Gu, outlines alternations in pain perception faced by people on the autism spectrum and how those changes can affect them in social functions. 1) Autism may increase sensitivity to pain
Research
Autistic children had normal plasma and urinary thiamine levels whereas plasma TPP concentration was decreased. The latter may be linked to abnormal tissue handling and/or absorption from gut microbiotaThe bacterial community which causes chronic diseases - one which almost certainly includes multiple species and bacterial forms. of TPP which warrants further investigation. Increased plasma protein dityrosine may reflect increased dual oxidase activity in response to change in mucosal immunity and host-microbe homeostasis. 2)
Epidemiology
The prevalence of autism in the United States has increased significantly over the past twenty years. Using information from state birth records and case records of patients affiliated with the California Department of Health Services, Bearman and colleagues estimate that approximately 25 percent of the increased prevalence of autism observed in California between 1992 and 2005 is due to changes in how autism is diagnosed.3)
Dr. Bearman and colleagues recently published that there are certain geographical areas of California where babies are more likely to develop autism (see right). The authors point out that localized “clusters” of autism suggests that environmental factors such as increased public awareness and local advocacy may play a role. However, clusters of disease may just as well suggest autism is caused by a communicable infection such as the slow-growing chronic infection described by the Marshall PathogenesisA description for how chronic inflammatory diseases originate and develop..
Evidence of infectious cause
Growing evidence exists to conclude that autism spectrum disorder is driven by microbial pathogens.
Unique microbial populations
Persistent co-infections are generally a sign of an immune system disabled by the Th1 pathogensThe community of bacterial pathogens which cause chronic inflammatory disease - one which almost certainly includes multiple species and bacterial forms.. It's telling to note that there remains no conclusive evidence for any single kind of virus always present in patients with autism.
- Patients with autism tend to suffer from severe gastrointestinal problems and have different bacteria in their GI tract. In a 2005 Paracho et al. study, the fecal flora of ASD patients contained a higher incidence of Clostridium histolyticum bacteria than that of healthy children.4)
- According to Nicolson et al.: “A large subset of ASD [autism spectrum disorder] patients shows evidence of bacterial and/or viral infections.” 5) He reports that his team found conclusive evidence of Mycoplasma ssp., Chlamydia pneunomiae, and human herpes virus-6 coinfections in ASD patients.
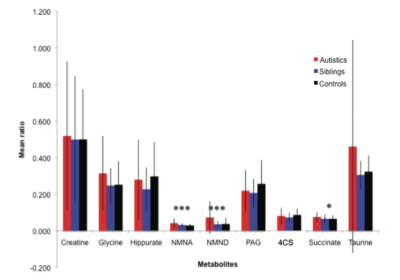
- Nicolson's team also showed that autistic children had several urinary metabolites that were highly significant as compared to controls (see right).6) This study confirms other work that children with ASD have unique microbial populations and further suggests that ASD could be clinically diagnosed using a urine test.
Other evidence
- Familial aggregationOccurrence of a given trait shared by members of a family (or community) that cannot be readily accounted for by chance. of other chronic inflammatory diseases – In one large-scale study, schizophrenia was more common among mothers and fathers of autistic children compared to controls. Depression and personality disorders were more common among case mothers but not fathers.7) A John's Hopkins study found that mothers with celiac disease and rheumatoid arthritis have higher incidence of having children with autism. A connection was also identified for children with a family history of type 1 diabetes.8)
- Autistic symptoms appear following infection reactivation – One paper described two cases of children who at first developed normally, but before the age of three developed autistic symptoms following the reactivation of a chronic oto-rhinolaryngologic infection“9)
- Autoantibodies – In a 2009 study, a significant proportion of autistic children harbored brain myelin basic protein autoantibodies and elevated levels of antibodies to measles virus and measles-mumps-rubella (MMR) vaccine.10) A second study found high levels of anti-nuclear antibodies in the blood serum of Egyptian autistic children.11) The Marshall Pathogenesis explains so-called “autoantibodies” as antibodies generated in response to pathogenic bacterial cells that have been destroyed as a result of an active immune response.
- Temporary remission of symptoms during fever – A Johns Hopkins research team has documented how children with ASD exhibit fewer characteristic autistic behaviors during fever, a change which was unrelated to fever severity.12) This provocative change in behavior may be due to the fact that acute infections such as those which cause fevers may temporarily delay immunopathologyA temporary increase in disease symptoms experienced by Marshall Protocol patients that results from the release of cytokines and endotoxins as disease-causing bacteria are killed.. In the absence of immunopathology, autistic children display less behaviors characteristic of autism and consistent with die-off of chronic bacteria.
- Prenatal infection and autism – A population-wide study from Denmark spanning two decades of births indicates that infection during pregnancy increases the risk of autism in the child. Hospitalization for a viral infection, like the flu, during the first trimester of pregnancy triples the odds. Bacterial infection, including of the urinary tract, during the second trimester increases chances by 40 percent.13)
- Read additional studies – PubMed studies that discuss the microbiology of autism
Patient interviews

autism, ADHD, depression, severe anxiety, chronic fatigue syndrome (CFS)
Read the interview
Interviews of patients with other diseases are also available.
Prodigies, autism, and the interactome
As described in Psychology Today, autism and being a prodigy are closely related:
Ruthsatz found that both the first-degree families of individuals with autism and the first-degree families of prodigies in her sample displayed three out of five common traits of autism: impaired social skills, impaired ability to switch attention, and heightened attention to detail. This intrigued her, so she decided to look for autism in her current sample of prodigies.
Lo and behold, while about one in every 88 children in the United States is diagnosed with autism, four out of the eight prodigies in the current study had family members who either had an autism diagnosis or had a first- or second-degree relative with an autism diagnosis. Additionally, three of the prodigies had already been diagnosed with autism, and as a group they showed higher levels of autistic traits compared with a control group consisting of people weren't prodigies (but scored only slightly higher than those with high-functioning autism, or Asperger's.
This may be a case where the exact interaction among microbes, known as the interactome, may contribute both to illness as well as exceptional cognitive abilities.
Read More
[PMID: 28452081] [PMCID: 5659957] [DOI: 10.1111/ejn.13598]
[PMID: 27667096] [DOI: 10.1080/10715762.2016.1239821]
[PMID: 19737791] [PMCID: 2800781] [DOI: 10.1093/ije/dyp261]
[PMID: 16157555] [DOI: 10.1099/jmm.0.46101-0]
[PMID: 17265454] [DOI: 10.1002/jnr.21203]
[PMID: 20337404] [DOI: 10.1021/pr901188e]
[PMID: 18450879] [DOI: 10.1542/peds.2007-2296]
[PMID: 19581261] [DOI: 10.1542/peds.2008-2445]
[PMID: 12478882] [DOI: 10.3109/15622970209150618]
[PMID: 19758536]
[PMID: 19135624] [DOI: 10.1016/j.pediatrneurol.2008.10.017]
[PMID: 18055656] [DOI: 10.1542/peds.2007-0360]
[PMID: 20414802] [DOI: 10.1007/s10803-010-1006-y]