Bias in observational epidemiological studies
It is arguably impossible to sufficiently control for the socioeconomic factors, which drive a person to participate in a therapy or take a supplement. The case of hormone replacement therapy (HRT) is instructive. For decades, researchers thought that HRT prevented disease, but it was ultimately shown that it caused it.
Studies of vitamin D's efficacy are especially fraught with challenges. For one, the secosteroid is palliative and the negative side effects can only be seen after decades of use. Also, people who take vitamin D are demonstrably different than those who don't. They almost always have a higher socioeconomic status.
Not all studies on vitamin D's efficacy are observational, but those that are may warrant a special amount of skepticism.
Hormone replacement therapy: a cautionary example
In a widely-studied example, numerous epidemiological studies as recently as 15 years ago showed that women who were taking combined hormone replacement therapy (HRT) also had a lower-than-average incidence of coronary heart disease (CHD), leading doctors to propose that HRT was protective against CHD. One researcher's comment at the time was typical:
Overall, the bulk of the evidence strongly supports a protective effect of estrogens that is unlikely to be explained by confounding factors.
Meir Stampfer, et al. 1)
There must have been some mistake, because this statement has been shown, conclusively, to be erroneous.
Controlled trials showed that HRT caused a small and significant increase in risk of CHD. Re-analysis of the data showed that women undertaking HRT were more likely to be from socio-economic groups ABC1, with better than average diet and exercise regimes. The two were coincident effects of a common cause, rather than cause and effect as had been supposed.2)
According to Gary Taubes, “The question of how many women may have died prematurely or suffered strokes or breast cancer because they were taking a pill that their physicians had prescribed to protect them against heart disease lingers unanswered. A reasonable estimate would be tens of thousands.”
One retrospective commentary, full of all the requisite browbeating, asked provocatively “Is this the death of observational epidemiology?”3)
People who supplement with vitamin D are demonstrably different
A number of epidemiological studies examining the efficacy of vitamin D are vulnerable in the same way the hormone replacement therapy studies are.
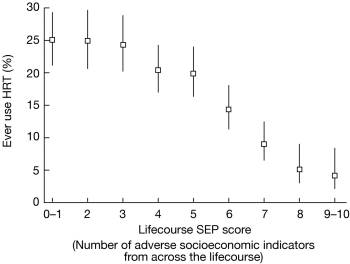
Studies in which a cohort is self-selecting can be fraught with error, especially when the groups are substantively different. The people who take vitamin D are different than those who don't. They tend to have more money, better education, and better health care, a well-documented pattern.
One recent British study is typical.4) The primary purpose of the study was to measure serum levels of 25-DThe vitamin D metabolite widely (and erroneously) considered best indicator of vitamin D "deficiency." Inactivates the Vitamin D Nuclear Receptor. Produced by hydroxylation of vitamin D3 in the liver. in middle aged white adults. The patient pool consisted of 7,437 people from the 1958 British birth cohort. Researchers stratified subjects by socioeconomic class. Socioeconomic status was assessed by using the Registrar General's occupational classification based on current or most recent occupation at age 42 and categorized as I and II (professional and managerial), III (skilled) nonmanual, III (skilled) manual, and IV and V (partly skilled and unskilled).
According to the results, subjects in the highest socioeconomic class were almost twice as likely to take cod liver, fish oil, or other supplements containing vitamin D as those in a lower class (p < 0.0001).
| Socioeconomic status | Percent taking vitamin D |
|---|---|
| I and II, professional and managerial | 19.6% |
| III, nonmanual | 18.4% |
| III, manual | 12.2% |
| IV and V, partially skilled and unskilled | 11.3% |
| Unclassified | 12.2% |
Even studies looking at rates of supplementation in countries where the practice is more widespread have noted this effect. In a study of the 1966 Northern Finland birth cohort, which consisted of 7,648 people, it's apparent that socioeconomic status correlates with the choice to give supplements containing vitamin D.5)
- 86% of mothers who follow health education gave their children vitamin D supplements as opposed to 79% who rarely or never did.
- 88% of professional mothers gave their sons and daughters vitamin D supplements as opposed to 74% of farmers' offspring.
- 87% of those with more than a basic education gave the supplement as opposed to 80% who had a basic or no education.
Unreliable research, Press releases
A systematic approach using statistical techniques to assess randomization outcomes can evaluate data integrity, in this case suggesting these RCT results may be unreliable. 6)
Dietary supplements industry press releases issued in response to clinical research findings are characterized by 'spin' that hypes results that are favourable to supplement use and denigrates results that are not.7)
[PMID: 1826173] [DOI: 10.1016/0091-7435(91)90006-p]
[PMID: 15166201] [DOI: 10.1093/ije/dyh124]
[PMID: 17344510] [DOI: 10.1093/ajcn/85.3.860]
[PMID: 15699498] [DOI: 10.1196/annals.1337.013]
[PMID: 27920281] [DOI: 10.1212/WNL.0000000000003387]
[PMID: 24992571] [PMCID: 4081644] [DOI: 10.1371/journal.pone.0101533]