
Table of Contents
Markers for Study Design
Direct detection of bacteria
- Now, this seems to be an interesting test. Inge
- The obvious question with this or any other test is how it works at picking up intracellular infections. –Paul
TLR2
Trevor mentioned this about reduced TLR2A receptor which is expressed on the surface of certain cells and recognizes native or foreign substances and passes on appropriate signals to the cell and/or the nervous system. expression as being a possible marker
Methods: Total BAL cells (cultured four or 24h in medium, or stimulated 24h with LPS) from 14 patients and six healthy subjects, sorted AMs from 22 patients (Lofgren's syndrome n=11) and 11 healthy subjects, and sorted CD4+ T cells from 26 patients (Lofgren's syndrome n=13) and seven healthy subjects, were included.
Using real-time PCR, the relative gene expression of IL-10, IL-12p35, IL-12p40, IL-23p19, CCR2, CCR7, iNOS, CXCL10, CXCL11, CXCL16, CCL18, CCL20, CD80, and CD86, and innate immune receptors TLR2, TLR4, and TLR9, was quantified in sorted AMs, and for selected genes in total BAL cells, while IL-17A was quantified in T cells.
Results: We did not find evidence of a difference with regard to alveolar macrophage M1/M2 polarization between sarcoidosis patients and healthy controls. TLR2 gene expression was significantly lower in sorted AMs from patients, particular in Lofgren's patients.
CCL18 gene expression in AMs was significantly higher in patients compared to controls. Additionally, the IL-17A expression was lower in Lofgren's patients'CD4+ T cells.
Conclusions: Overall, there was no evidence for alveolar macrophage polarization in sarcoidosis.
However, there was a reduced TLR2 mRNA expression in patients with Lofgren's syndrome, which may be of relevance for macrophage interactions with a postulated sarcoidosis pathogen, and for the characteristics of the ensuing T cell response.
Author: Maria WikenFarah IdaliMuntasir Abo Al HayjaJohan GrunewaldAnders EklundJan Wahlstrom Credits/Source: Respiratory Research 2010, 11:121
Endotoxins
Intensive Care Med. 2002 Jul;28(7):824-33. Epub 2002 May 30. Clinical implications of antibiotic-induced endotoxin release in septic shock. Lepper PM, Held TK, Schneider EM, Bölke E, Gerlach H, Trautmann M. Source Dept. of Medical Microbiology and Hygiene, University Hospital, Steinhövelstr. 9, 89075 Ulm, Germany. Abstract Antibiotic-induced release of bacterial cell wall components can have immediate adverse effects for the patient. This article reviews the data on endotoxin release after initiation of antibiotic therapy and its role in the pathogenesis of sepsis and septic shock. Antibiotics differ in their potential to liberate endotoxins from bacterial cell walls. When used for treatment of systemic Gram-negative infection, some classes of beta-lactam antibiotics lead to markedly increased levels of free endotoxins while treatment with carbapenems and aminoglycosides produces relatively low amounts of endotoxins. Antibiotics that induce the formation of long, aberrant bacterial cells before effectively killing the microorganisms show the highest degree of endotoxin liberation. There is increasing evidence from animal models and clinical studies of sepsis that the antibiotic-mediated release of biologically active cell wall components derived from Gram-positive, Gram-negative or fungal organisms is associated with a rapid clinical deterioration.
PMID: 12122518
Hi Greg,
I have an idea for a study. These days we talk about IP as if it's two components: inflammationThe complex biological response of vascular tissues to harmful stimuli such as pathogens or damaged cells. It is a protective attempt by the organism to remove the injurious stimuli as well as initiate the healing process for the tissue. and endotoxins. Showing heightened inflammation in patients with inflammatory diseases doesn't accomplish anything, but looking for endotoxins might. To date, a lot of the endotoxin research appears to be concentrated on these topics: - severe sepsis - nosocomial infections - effect of beta-lactam antibiotics - etc.
That I can see, nobody has thought about measuring endotoxins when chronic pathogens are killed, because nobody has been able to kill pathogens with any regularity.
I was talking to an ER doctor the other day, and he was saying that endotoxins tend to be species-specific, so I should be looking to measure levels of the protein to which endotoxins binds – which I believe would be lipopolysaccharide binding protein (LBP). Not all of the MP pathogens are gram-negative and have a cell wall, but wouldn't at least some meet that description? Otherwise, why even blame endotoxins?
If you went with the LBP kit I link to below, you could get 96 tests for ~$900. I'm not sure if you can do them one at a time or all at once. You could do a cross-sectional study: 48 on the MP vs. 48 not on the MP. Or, you could do a before starting the MP and after. You could then correlate endotoxin load with symptom severity.
Of course, you would need a lab to run this test.
Anyway, I wonder if you (or someone) could show that the MP increases serum bioavailability of endotoxins. If you did, that would be a substantial contribution to medicine.
Best, Paul
Begin forwarded message:
From: Paul Albert paa2013@med.cornell.edu Date: October 30, 2009 5:23:59 PM EDT To: m.trautmann@klinikum-stuttgart.de, philipp.lepper@insel.ch Subject: measurement of endotoxins
Dear Drs. Lepper and Trautmann,
I recently read your excellent 2002 review, “Clinical Implications of Antibiotic-Induced Endotoxin Release in Septic Shock.” (Attached for your convenience.)
I am on a team which is in the process of designing a study protocol in which patients will be administered a multi-year antibiotic-based therapy in order to eradicate the microbes we believe may be driving ankylosing spondylitis. In a pilot study, we have been able to consistently induce fever and other symptoms consistent with mild antibiotic-induced endotoxemia, which suggests a Jarisch-Herxheimer reaction. Our protocol uses rotating combinations of sub-inhibitory antibiotics: minocycline, clindamycin, and azithromycin. We're not sure what species are being killed or if they're predominantly gram-negative or gram-positive.
In your review, you mention that it's possible to measure endotoxins via “chromogenic Limulus amoebocyte lysate (LAL) assay.” Then you go on to talk about the various complications associated with LAL assays.
I've also read about tests which measure lipopolysaccharide binding protein (LBP). For example: https://www.cellsciences.com/content/p-detail.asp?rowid=4392&buy=4392
If we want to demonstrate that our therapy increases serum bioavailability of endotoxins (which suggests bacteria die-off) what marker and/or assay, would you recommend?
Regards, Paul Albert
Lipopolysaccharides, and indeed the other cell-wall components, are probably not likely to yield useful results in our cohort. These proteins are not expressed in the L-formDifficult-to-culture bacteria that lack a cell wall and are not detectable by traditional culturing processes. Sometimes referred to as cell wall deficient bacteria.. However, the target of TLR2 is of interest to me, as are a number of other emerging inflammatory markers. At the conference yesterday there were two very good presentations on innate and adaptive immunity. Many of the endotoxins are described in that set of slides, including the antibodies (which I would also be interested in tracking). I will try to put the presentations online within the next few days…
Trevor
Hi Dr. Lepper,
Sorry for my tardiness in response. I was on quite a long vacation!
We were hoping to use blood serum in case you don't remember in patients with ankylosing spondylitis. Are there any assays that are not time-consuming? I'm not sure we have the resources for time/money-intensive approaches.
thanks,
Paul Albert Weill Cornell Medical College 212.746.7541
On Nov 30, 2009, at 6:05 AM, Philipp M. Lepper wrote:
Dear Dr. Albert,
please excuse the delay. Could you specify your question a bit regarding what material you intend to use (serum, joint effusion…).
There are several assays availbale - however it depends also on the resources you have as some assays are timeconsuming.
Best regards Philipp Lepper
– Dr. Philipp M. Lepper Dept. of Pneumology Infection and Immunity Group University Hospital of Bern (Inselspital) CH-3010 Bern Switzerland Tel.: ++41 (0) 31 632 9832 Fax: ++41 (0) 31 632 1404 E-mail: philipp.lepper@insel.ch
Antimicrobial peptides
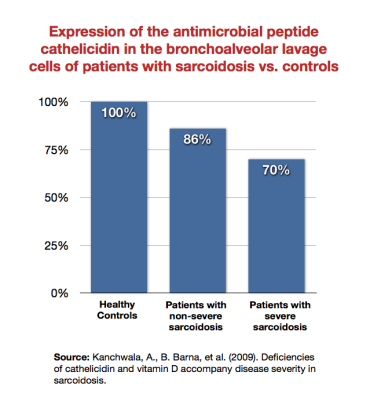
- Kanchwala et al. showed that patients with sarcoidosis expressed the antimicrobial peptide cathelicidin Family of antimicrobial peptides found primarily in immune cells and transcribed by the Vitamin D Receptor. less than healthy subjects, and that sicker sarcoidosis patients expressed it least of all.1) Wiken et al. showed that there was a reduced TLR2 mRNA expression in patients with Lofgren's syndrome (a type of acute sarcoidosis).2) Note that TLR2 (which the Marshall PathogenesisA description for how chronic inflammatory diseases originate and develop. theorizes is downregulated in autoimmune disease states) is expressed by the VDRThe Vitamin D Receptor. A nuclear receptor located throughout the body that plays a key role in the innate immune response..
- Wang et al. have demonstrated in Crohn's patients a decline in expression of key antimicrobial peptidesBody’s naturally produced broad-spectrum antibacterials which target pathogens. including cathelicidin and Beta-defensin An antimicrobial peptide found primarily in immune cells and transcribed by the Vitamin D Receptor.-2.3) Consistent with the Marshall Pathogenesis, the group points to the Vitamin D ReceptorA nuclear receptor located throughout the body that plays a key role in the innate immune response. as being important in Crohn's patients.
Respirology. 2011 May;16(4):611-6. doi: 10.1111/j.1440-1843.2011.01924.x. Vitamin D, innate immunityThe body's first line of defense against intracellular and other pathogens. According to the Marshall Pathogenesis the innate immune system becomes disabled as patients develop chronic disease. and outcomes in community acquired pneumonia. Leow L, Simpson T, Cursons R, Karalus N, Hancox RJ. Source Respiratory Research Unit, Waikato Hospital Department of Molecular Genetics, University of Waikato, Hamilton Department of Preventive and Social Medicine, University of Otago, Dunedin, New Zealand. Abstract BACKGROUND AND OBJECTIVE: Vitamin D regulates the production of the antimicrobial peptides cathelicidin and beta-defensin-2, which play an important role in the innate immune responseThe body's first line of defense against intracellular and other pathogens. According to the Marshall Pathogenesis the innate immune system becomes disabled as patients develop chronic disease. to infection. We hypothesized that vitamin D deficiency would be associated with lower levels of these peptides and worse outcomes in patients admitted to hospital with community acquired pneumonia.
METHODS: Associations between mortality and serum levels of 25-hydroxyvitamin D, cathelicidin and beta-defensin-2 were investigated in a prospective cohort of 112 patients admitted with community acquired pneumonia during winter.
RESULTS: Severe 25-hydroxyvitamin D deficiency (<30nmol/L) was common in this population (15%) and was associated with a higher 30-day mortality compared with patients with sufficient 25-hydroxyvitamin D (>50nmol/L) (odds ratio 12.7, 95% confidence interval: 2.2-73.3, P=0.004). These associations were not explained by differences in age, comorbidities, or the severity of the acute illness. Neither cathelicidin nor beta-defensin-2 levels predicted mortality, although there was a trend towards increased mortality with lower cathelicidin (P=0.053). Neither cathelicidin nor beta-defensin-2 levels correlated with 25-hydroxyvitamin D.
CONCLUSIONS: 25-hydroxyvitamin D deficiency is associated with increased mortality in patients admitted to hospital with community acquired pneumonia during winter. Contrary to our hypothesis, 25-hydroxyvitamin D levels were not associated with levels of cathelicidin or beta-defensin-2.
© 2011 The Authors. Respirology © 2011 Asian Pacific Society of Respirology.
PMID: 21244571
Curr Opin Hematol. 2002 Jan;9(1):18-22. Cathelicidins Family of antimicrobial peptides found primarily in immune cells and transcribed by the Vitamin D Receptor.: a family of endogenous antimicrobial peptides. Lehrer RI, Ganz T. Source Department of Medicine, Molecular Biology Institute, University of California at Los Angeles, Los Angeles, California, USA. rlehrer@mednet.ucla.edu Abstract The cytoplasmic granules of mammalian neutrophils contain several antimicrobial peptides. Some, like defensins, are fully processed before storage, whereas others are stored as precursors that require additional processing. Cathelicidins are bipartite molecules with an N-terminal cathelin domain and an antimicrobial C-terminal domain. Humans apparently have only one cathelicidin gene. Its product, hCAP-18, is present in the secondary (specific) granules of neutrophils, and its C-terminal antimicrobial peptide, LL-37, is liberated by proteinase 3 coincident with degranulation and secretion. Many nonmyeloid tissues also express hCAP-18, including epididymis, spermatids, keratinocytes, epithelial cells, and various lymphocytes. LL-37 stimulates chemotaxis, acting via the formyl peptide-like receptor-1. The structurally diverse cathelicidin-derived antimicrobial peptides of animals provide interesting models for pharmaceutical development. PR-39, a proline-rich porcine cathelicidin, has shown efficacy in limiting myocardial damage after experimental ischemia in rodent models. Porcine protegrins are in stage III clinical trials to prevent oral mucositis caused by radiation or chemo-therapy.
PMID: 11753073
Arch Med Res. 2011 Apr;42(3):189-94. Human β-Defensin-2 Induction in Nasal Mucosa after Administration of Bacterial Lysates. Guaní-Guerra E, Negrete-García MC, Montes-Vizuet R, Asbun-Bojalil J, Terán LM. Source Superior School of Medicine, National Polytechnic Institute (ESM-IPN), Mexico City, Mexico; Department of Immunogenetics, National Institute of Respiratory Diseases (INER), Mexico City, Mexico. Abstract BACKGROUND AND AIMS: The airway epithelium produces antimicrobial peptides (AMPs) that prevent colonization of host tissues by a wide range of pathogens. Human β-defensin 2 (hBD-2) is one of the most well-documented AMPs in humans. Several bacterial products can induce production of this peptide. Bacterial immunostimulants containing bacterial lysates have long been used in the treatment of respiratory infections, but their effects on hBD-2 release have not been investigated. We undertook this study to induce production of hBD-2 after stimulation of the nasal mucosa with bacterial lysates.
METHODS: A nasal lavage (NL) was performed in 12 healthy volunteers under basal conditions and after a nasal challenge with separate and subsequent stimuli with either bacterial lysates (20 million), cholecalciferol (400 IU), or sham-challenge with glycerol plus isotonic saline solution. Immunohistochemistry was performed in nasal biopsies 48 h after stimulation with bacterial lysates to identify the presence of hBD-2.
RESULTS: Increased levels of hBD-2 (4668.99 ± 2829.33 pg/mL) were measured with ELISA in NL fluids following bacterial challenge. However, hBD-2 concentrations were below the limit of detection in NL fluids at baseline and after the administration of cholecalciferol or the sham-challenge. Through immunohistochemistry, hBD-2 was predominantly localized to the epithelium.
CONCLUSIONS: hBD-2 can be induced in the nasal mucosa after administration of bacterial lysates. Stimulation of the innate immune system to produce hBD-2 could be used to prevent or even treat infections caused by respiratory pathogens.
Copyright © 2011 IMSS. All rights reserved.
PMID: 21722813
Autoantibodies
J AutoimmuneA condition or disease thought to arise from an overactive immune response of the body against substances and tissues normally present in the body Dis. 2005 May 25;2:5. Evaluation of autoantibodies to common and neuronal cell antigens in Chronic Fatigue Syndrome. Vernon SD, Reeves WC. Source Division of Viral and Rickettsial Diseases, National Center for Infectious Diseases, Centers for Disease Control and Prevention, Atlanta, Georgia 30333, USA. svernon@cdc.gov Abstract People with chronic fatigue syndrome (CFS) suffer from multiple symptoms including fatigue, impaired memory and concentration, unrefreshing sleep and musculoskeletal pain. The exact causes of CFS are not known, but the symptom complex resembles that of several diseases that affect the immune system and autoantibodies may provide clues to the various etiologies of CFS. We used ELISA, immunoblot and commercially available assays to test serum from subjects enrolled in a physician-based surveillance study conducted in Atlanta, Georgia and a population-based study in Wichita, Kansas for a number of common autoantibodies and antibodies to neuron specific antigens. Subsets of those with CFS had higher rates of antibodies to microtubule-associated protein 2 (MAP2) (p = 0.03) and ssDNA (p = 0.04). There was no evidence of higher rates for several common nuclear and cellular antigens in people with CFS. Autoantibodies to specific host cell antigens may be a useful approach for identifying subsets of people with CFS, identify biomarkers, and provide clues to CFS etiologies.
PMID: 15916704 [PubMed
Int J Mol Med. 2003 Aug;12(2):225-30. Autoantibodies against muscarinic cholinergic receptor in chronic fatigue syndrome. Tanaka S, Kuratsune H, Hidaka Y, Hakariya Y, Tatsumi KI, Takano T, Kanakura Y, Amino N. Source Department of Laboratory Medicine, Osaka University Graduate School of Medicine (D2), Suita-shi, Osaka 565-0871, Japan. tanaka@labo.med.osaka-u.ac.jp Abstract The disturbance of the central nervous system and immunological abnormalities have been suggested in patients with chronic fatigue syndrome (CFS). We focused on immunological abnormalities against neurotransmitter receptors in CFS. Using a sensitive radioligand assay, we examined serum autoantibodies to recombinant human muscarinic cholinergic receptor 1 (CHRM1), mu-opioid receptor (OPRM1), 5-hydroxytryptamine receptor 1A (HTR1A), and dopamine receptor D2 (DRD2) in patients with CFS (n=60) and results were compared with those in patients with autoimmune disease (n=33) and in healthy controls (n=30). The mean anti-CHRM1 antibody index was significantly higher in patients with CFS (p<0.0001) and autoimmune disease (p<0.05) than that in healthy controls, and positive reaction was found in 53.3% of patients with CFS. Anti-OPRM1 antibodies, anti-HTR1A antibodies, and anti-DRD2 antibodies were found in 15.2, 1.7, and 5.0% of patients with CFS, respectively. Anti-nuclear antibodies were found in 56.7% (34/60) of patients with CFS, but anti-nuclear antibody titers did not correlate with the activities of the above four autoantibodies. The patients with positive autoantibodies to CHRM1 had a significantly higher mean score (1.81) of 'feeling of muscle weakness' than negative patients (1.18) among CFS patients (p<0.01). Higher scores on 'painful node', 'forgetfulness', and 'difficulty thinking' were also found in CFS patients with anti-CHRM1 antibodies but did not reach statistical significance. In conclusion, autoantibodies to CHRM1 were detected in a large number of CFS patients and were related to CFS symptoms. Our findings suggested that subgroups of CFS are associated with autoimmune abnormalities of CHRM1.
PMID: 12851722
Clin Endocrinol (Oxf). 1997 Apr;46(4):467-72. High incidence of positive autoantibodies against thyroid peroxidase and thyroglobulin in patients with sarcoidosis. Nakamura H, Genma R, Mikami T, Kitahara A, Natsume H, Andoh S, Nagasawa S, Nishiyama K, Chida K, Sato A, Yoshimi T. Source Department of Internal Medicine, Hamamatsu University School of Medicine, Japan. Abstract OBJECTIVE: Although abnormalities of the humoral immune system, such as increased immunoglobulin production, are known in sarcoidosis, the relationship between sarcoidosis and autoimmune disorders in uncertain. We studied the incidence of thyroid autoantibodies and the prevalence of Hashimoto's thyroiditis in patients with sarcoidosis.
PATIENTS AND MEASUREMENTS: Sixty-two patients with pulmonary sarcoidosis, diagnosed by a combination of clinical, radiographic and histological findings were studied. As controls, three groups of subjects aged 40 and over without a known history of thyroid disease (60 patients with pulmonary diseases other than sarcoidosis, 88 hospital employees and 82 company workers), were also analysed. Antibodies against thyroid peroxidase (TPO-Ab) and purified thyroglobulin (Tg-Ab) were measured by radioimmunoassay and antibodies against microsomal antigen (MCHA) and thyroglobulin (TGHA), by haemagglutination.
RESULTS: Seventeen of 62 patients (27.4%) had either positive TPO-Ab or Tg-Ab or both. All the patients with positive thyroid autoantibodies were of middle or advanced age, and the incidence of positive TPO-Ab/Tg-Ab in patients with sarcoidosis aged 40 and over was 54.5% in males, 32.4% in females and 37.8% overall. The prevalence was significantly higher in males compared to age-matched control males (0-7.7% in the controls), and in female patients was twice that found in controls (11.8-16.3%). Seven patients had Hashimoto's thyroiditis, indicating that the prevalence was 11-3%, and much higher than that previously reported.
CONCLUSIONS: The data show a remarkably high incidence of thyroid autoantibodies in patients of middle of advanced age with sarcoidosis, especially in males, and a higher prevalence of Hashimoto's thyroiditis than in previous reports.
PMID: 9196610
Bacterial signaling
Interesting TED lecture on bacterial communication via specialized chemicals - both species specific and generic.
https://www.ted.com/index.php/talks/bonnie_bassler_on_how_bacteria_communicate.html
So…if a biofilm A structured community of microorganisms encapsulated within a self-developed protective matrix and living together. can excrete a chemical marker, whose concentration “tells” the collection of bacteria when to become mobile and “invade”, it's a small stretch to include excreted markers that encourage conversion to invasive CWD forms, or cysts (Borrelia), or migration to low O2 regions, or migration to heart/lung/CNS tissue, etc..
Chris
Cytokines
Interleukin-6
Full text here
Clin Biochem. 2010 Nov;43(16-17):1309-14. Epub 2010 Jul 23. Correlation of a multi-cytokineAny of various protein molecules secreted by cells of the immune system that serve to regulate the immune system. panel with clinical disease activity in patients with rheumatoid arthritis. Milman N, Karsh J, Booth RA. Source Faculty of Medicine, University of Ottawa, 451 Smyth Rd., Ottawa ON, Canada K1H 8M5. Abstract OBJECTIVE: Explore the potential use of a cytokine panel as biochemical markers of disease activity in rheumatoid arthritis (RA) patients.
DESIGN AND METHODS: 57 adult RA patients were assessed using five validated clinical disease activity tools: Health Assessment Questionnaire (HAQ), standard 28-joint Disease Activity Score (DAS28), DAS28 using C-reactive protein (DAS28-CRP), Clinical Disease Activity Index (CDAI), and Simple Disease Activity Index (SDAI). Plasma cytokine levels (IL-2, IL-4, IL-6, IL-8, IL-10, VEGF, IFN-γ, TNF-α, IL1α, IL1β, MCP1, and EGF) were measured in 47 of the 57 patients and correlated with clinical indicators.
RESULTS: We found significant correlations between plasma levels of IL-6 and all clinical measures of disease activity; Spearman coefficients (p values) were: HAQ: 0.347(0.017); DAS28: 0.409(0.005); DAS-CRP: 0.378(0.011); CDAI: 0.312(0.033); SDAI: 0.310(0.039); ESR: 0.448(0.002); and CRP: 0.513(0.001). IFN-γ also correlated with DAS-CRP: 0.309(0.039) and SDAI: 0.301(0.044). Furthermore, the levels of IL-6 and IFN-γ increased significantly with worsening disease, as defined by the European League Against Rheumatism (EULAR) classification of disease activity.
CONCLUSION: A significant correlation between plasma levels of IL-6 and clinical disease activity in patients with RA suggests a future role of IL6 as a disease activity marker.
Copyright © 2010. Published by Elsevier Inc.
PMID: 20655893
Antigens in blood using amplification, arrays
Despite the great strides medicine has made in the past century, diagnosing infectious disease remains a difficult – and often impossible – task. One major barrier in diagnosis is knowing what to look for. Which of the millions of potentially antigenic products that a pathogen makes can actually be found in bodily fluids and used as indicators of infection? After all, not every protein or polysaccharide belonging to a pathogen can make it into a handy sample of urine or blood, so which CAN we use?
A study in mBio this week brings us a little closer to identifying those antigens that could be used in diagnostics. Using a technique they call In vivoA type of scientific study that analyzes an organism in its natural living environment. Microbial Antigen Discovery (InMAD), Nuti et al. were able to amplify the small signals present in an infected mouse’s blood by purifying serum samples and using them to immunize another mouse. Serum from this second mouse contains antibodies for the bacterial components in the blood of the first mouse. They used this serum to probe blots of bacterial lysates and bacterial proteome arrays. The spots on the blot or the array that lit up indicate which antigens the mouse immune system reacts to – precisely the antigens that could be targeted in an assay. Click on the source link above to read more on mBio's blog, mBiosphere…
Contacts
Comments
I am waiting to see a detailed study plan, including a rationale which is likely to get through an IRB. Your current letter speaks about “endogenous antimicrobials” while your previous letter spoke about “cathelicidin.” There is a difference, and we need to make sure we get all this stuff worked out before jumping in, feet-first. We need to understand what we are measuring.
How do we do 'antimicrobial' assays? Is there an FDA-approved test for them? If not, I think we will need an IRB approval, and a test which is definitive. Maybe the rules are different overseas, in which case we need to understand that difference, and figure out how to comply with those rules.
Trevort
References
[PMID: 19948723] [PMCID: 2807280] [DOI: 10.1074/jbc.C109.071225]

