
Table of Contents
Dosage and administration of olmesartan (Benicar)
It is imperative that patients on the Marshall Protocol (MP) take regular doses of olmesartan medoxomil (the brand name of which is Benicar), a medication for which there is no substitute. Olmesartan has an highly safe track record. MP patients are required to take 40mg of olmesartan every six hours – that is, equally spaced doses, four times a day – with or without food. Patients who take olmesartan once a day are not doing the MP. Do not ramp or gradually increase olmesartan.
In cases where a dose is missed, patients may take an extra olmesartan as soon as possible and/or sublingually. When severe immunopathology strikes or in the case of an acute emergency, patients may increase the frequency of olmesartan to up to six times day. Another option is to take a dose of 60mg.
MP patients may want to keep at least one month of extra olmesartan on hand.
Dosing frequency
These charts illustrate how frequent and consistent dosing smooths out the concentration levels. This is thought to be the reason that frequent and consistent dosing often helps to stabilize or resolve intolerable symptoms.
80 mg single dose vs 6 hourly dosing
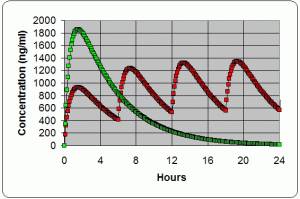
- Green line is serum (blood) concentrations of a single dose of 80 mg of Benicar over a 24 hour period.
Following a dosing schedule of taking the Benicar every 24 hours allows the serum concentrations to be near or at zero for the second half of the day.
- Red line is serum concentrations when taking 40 mg of Benicar every 6 hours over a 24 hour period.
Following a dosing schedule of taking the Benicar every 6 hours keeps the serum concentration from falling much below 600 ng/ml at all times. This seems to be adequate for managing typical levels of symptoms and the peaks at around 1200-1400 ng/ml may be periods of the greatest symptom palliation and/or immune stimulation.
4 hourly compared to 6 hourly dosing
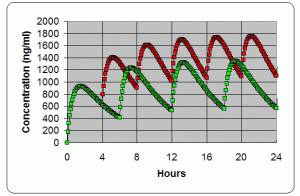
- Green line of data points is serum concentrations when taking 40 mg every 6 hours over a 24 hour period
- Red line of data points is serum concentrations when taking 40 mg every 4 hours over a 24 hour period
Following a dosing schedule of taking the Benicar every 4 hours keeps the serum concentration from falling below 1000 ng/ml at all times. This often proves to be more helpful for managing high levels of symptoms with greater symptom palliation.
When to take olmesartan
Under most circumstances, patients are expected to take 40mg of olmesartan every six hours for a total of 160mg of olmesartan in any 24-hour period.
If necessary, patients may need to set an alarm clock. When to take olmesartan is a question of personal preference and convenience. Here are a few suggestions:
- 6am, noon, 6pm, 12am
- 11pm, 7am, 12pm, 5pm (if one gets a lot of light during the day)
- 3am, 9am, 3pm, 9pm (ideal if one can fall back asleep)
It is usually okay to take olmesartan with or without other medications. Patients should consult their physician to see if there are any interactions to be concerned about between olmesartan and other medications. Usually, there are not.
It is okay to take olmesartan with or without food. Benicar tablets taken without food reach maximum concentration in 90 minutes. Sankyo, the manufacturer of Benicar, has shown that this time increases to 3-4 hours on a full stomach. Patients may want to be aware that if they vary whether they take olmesartan with or without a meal, they may want to adjust the timing of their dose accordingly.
Some have found that olmesartan seems to absorb more quickly by breaking the tablet in two to disrupt the microcoating and/or taking it with a hot drink (e.g. weak tea).
Alternative dosages
There is no evidence that patients who weigh more than average need to take additional olmesartan.
Dosing in response to strong immunopathology
When immunopathology becomes intolerable, one of the strategies for managing immunopathology is to take an extra 40mg of olmesartan sublingually. If intolerable symptom(s) persist, increase oral olmesartan to every three to fours hours around the clock, a dose which is safe. This schedule may be continued until symptoms are tolerable.
A smaller dose taken more frequently such as 20mg every two, three, or four hours may keep symptoms more tolerable. Some very symptomatic patients find they feel best taking 20mg of Benicar every three hours during the day and then 40mg at bedtime with the next dose six hours later. A typical schedule would be 20mg at 6am, 9am, noon, 3pm, 6pm, 9pm and then 40mg at midnight. That would be equivalent to 40mg every six hours or 160mg in a 24-hour period.
Do not ramp olmesartan
If possible, patients should not ramp up doses of olmesartan. Gradually increasing olmesartan only prolongs the adjustment period to the medication.
The olmesartan blockade dramatically lowers 1,25-D quickly, by as much as half in just two weeks. This rapid change causes a shift in many other hormones with resulting neurological type symptoms, such as photosensitivityAbnormal sensitivity to sunlight and bright lights. Also referred to as "sun flare" or "light flare.", fatigue, headache, irritability, sleep disturbances, brain fogThe loss of intellectual functions such as reasoning; memory loss; and other neurological abilities that is severe enough to interfere with daily functioning., etc. Rapid fluctuations of 1,25-D at any level can produce these symptoms.
When patients start at low or intermittent doses of olmesartan, they are making this adjustment especially difficult because the level of 1,25-D is allowed to fluctuate even more at points in time when the blockade is lost after the first six to eight hours. On the other hand, patients who put in a complete olmesartan blockade in place on day one with the recommended dose of 40mg every six hours will adjust to the new lower 1,25-D level within a couple weeks.
If one's physician insists on ramping a new patient's dose, ask to ramp up quickly, increasing by 40mg each day.
Conversely, patients who wish to discontinue olmesartan should decrease its use gradually and, if patient safety is an issue, not in an urgent care situation. Discontinuing olmesartan can have serious adverse results.
Alternative administration
Crushing olmesartan
Crushing Benicar and placing it in a capsule might increase the speed and efficiency of intestinal absorption, particularly in patients who have gastrointestinal malabsorption problems. For those folks, crushing might result in a higher tissue concentration and a more consistent Benicar blockade.
Crushing would not increase the potency of Benicar because it would still be subject to the same gastric and intestinal enzymes and it would still be metabolized by the liver. Crushed Benicar would also present the same stimulus as a noncrushed tablet to the intestinal tract of someone with food allergies. The assumption that crushing Benicar changes its properties to cause it to be more effective is speculation, something we discourage. We don't believe there is any pharmaceutical evidence that routine crushing of Benicar is necessary.
Sublingual administration
There are two situations in which patients may want to consider sublingual administration: if a dose is missed and in cases of strong immunopathology or exposure to light. With sublingual administration, a patient chews a tablet of olmesartan and places it underneath the tongue where it gets absorbed into the mucous membrane and passes into the bloodstream. Note that the FDA has not approved sublingual use of olmesartan and it is uncertain what effect its routine use would have on local soft tissues and tooth enamel.
Handling missed doses
The olmesartan blockade is lost if it has been longer than eight hours since the last dose. Patients who missed a dose should take 40mg immediately sublingually. Staying on schedule with olmesartan is important but if one fails, there is no need to panic. The inflammatory blockade will be reestablished in a day or two. Patients who aren't sure if they took their olmesartan dose can wait to see if they feel worse as the blockade dissipates and then take they dose. Or, they can take a half dose sublingually as an “insurance policy” and then resume their usual schedule. It will not hurt to take extra olmesartan.
Many patients on the MP have brain fog or memory impairment. It's important for them to develop a reliable system for remembering to take olmesartan.

