Forms and structure of vitamin D
All forms of vitamin D are secosteroids, sharing a close structural and functional resemblance to steroids. The full implications of a “vitamin” acting as a steroid has yet to be fully appreciated by many in the research community. The overlap between steroids and secosteroids is key to understanding the Marshall Pathogenesis. It explains how this “vitamin” can exert short-term palliative effects and long-term harm. Patients on the MP are advised to avoid consuming vitamin D, because of its immunomodulatory effects.
Summary of different forms
| Name | Source / How created | Description and function | Other names |
|---|---|---|---|
| 7-dehydrocholesterol | a cholesterol precursor | biologically inactive | previtamin-D3 |
| vitamin D2 | created by plants and fungi | ergocholecalciferol | |
| vitamin D3 | two sources: made in the skin when exposed to light; fish and meat | cholecalciferol; activated 7-dehydrocholesterol | |
| 25-D | produced by hydroxylation of vitamin D3 in the liver | inactivates the vitamin D nuclear receptor; widely (and erroneously) considered best indicator of vitamin D “deficiency” | 25-hydroxyvitamin D; calcidiol; calcifediol |
| 1,25-D | 25-D is further hydroxylated in the kidneys and infected macrophages by the enzyme 1-alpha-hydroxylase | primary biologically active vitamin D hormone; activates the vitamin D nuclear receptor | 1,25-dihydroxycholecalciferol; 1,25-dihydroxyvitamin D; calcitirol |
Vitamin D is a secosteroid
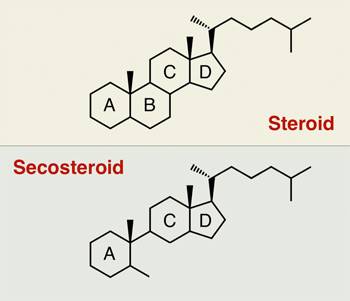
All forms of vitamin D belong to a family of lipids called secosteroids. Secosteroids are very similar in structure to steroids except that two of the B-ring carbon atoms of the typical four steroid rings are not joined, whereas in steroids they are.
The levels of each of the vitamin D metabolites are affected by a complex network of feedback mechanisms involving multiple enzymes and receptors, indicating vitamin D is regulated more like a steroid than a nutrient.
In the published literature, researchers sometimes distinguish between “steroid” and “secosteroid,” but not always.1) 2)
This failure to discriminate is less an indication of sloppy research and more a testament to how vitamin D behaves. The vitamins D act very much like steroids, binding nuclear receptorsIntracellular receptor proteins that bind to hydrophobic signal molecules (such as steroid and thyroid hormones) or intracellular metabolites and are thus activated to bind to specific DNA sequences which affect transcription. and modulating the immune response. Not only that, there's growing evidence that vitamin D causes adverse side effects like chronic disease over the long term as do anabolic steroids and corticosteroids.
[PMID: 10052453] [DOI: 10.1016/s0092-8674(00)80655-8]
[PMID: 12528991] [DOI: 10.2174/1389450033347118]