Presentation - Olmesartan overcomes antibiotic resistance, inducing recovery from advanced autoimmune disease
Type: Conference presentation
Presenter: Trevor Marshall, PhD
Conference: 7th International Congress on Autoimmunity
Location: Ljubljana, Slovenia
Date: May 2010
Abstract
Although early-stage autoimmune disease often succumbs to antibiotic therapy, antibiotics appear to lose utility as disease progresses. Recent sequencing of microbial DNA has confirmed that some pathogens ensure their persistence by reducing expression of, and transcription by, the VDRThe Vitamin D Receptor. A nuclear receptor located throughout the body that plays a key role in the innate immune response. Nuclear ReceptorIntracellular receptor proteins that bind to hydrophobic signal molecules (such as steroid and thyroid hormones) or intracellular metabolites and are thus activated to bind to specific DNA sequences which affects transcription., which is at the heart of the human innate immune system. Only in Homo sapiens is the VDR responsible for expression of the Cathelicidin Family of antimicrobial peptides found primarily in immune cells and transcribed by the Vitamin D Receptor. anti-microbial peptide, the primary defense of the intra-phagocytic innate immune system. The VDR is also responsible for expression of TLR2A receptor which is expressed on the surface of certain cells and recognizes native or foreign substances and passes on appropriate signals to the cell and/or the nervous system. and TACO and a number of other endogenous anti-microbials. Pathogens already known to persist by dysregulating the VDR include EBV, Mycobacteria, Borrelia and HIV. Antibacterial therapy is difficult, as the diseased VDR cannot be simply restored by Vitamin D metabolites, as it can in healthy individuals. The drug OlmesartanMedication taken regularly by patients on the Marshall Protocol for its ability to activate the Vitamin D Receptor. Also known by the trade name Benicar. functions as a VDR agonistA substance such as olmesartan (Benicar) or 1,25-D which activates the Vitamin D Receptor and transcribes the genes necessary for a proper innate immune response., restoring enough immune function for patients to again become responsive to bacteriostatic antibiotics. Indeed, care must be exercised to ensure the resulting cytokineAny of various protein molecules secreted by cells of the immune system that serve to regulate the immune system.-storm does not become life-threatening. VDR dysfunction results in ripple-down effects on the Thyroid, Glucocorticoid, Androgen and Progesterone receptors, which often return to normal in earlier years of the recovery process. New in silicoExperiment technique performed on computer or via computer emulation. research methodologies, including sequencing, modeling, and molecular-dynamics, have become essential tools in developing our understanding of the metagenomic microbiotaThe community of bacterial pathogens including those in an intracellular and biofilm state which cause chronic disease. which drives autoimmune disease, and how it interacts with the human genomes transcription and DNA repair mechanisms. An accurate model of disease processes is the essential factor in quickly moving these discoveries from bench to bedside.
Transcript
#1 Introduction
Thank you very much. For those of you who were present at the autoimmunity congress at Singapore would have remembered perhaps a very animated question and answer session between myself and Yehuda1) there on the issue of vitamin D. And in particular, whether you would want to supplement vitamin D in autoimmune conditions.
As I was putting together this presentation I thought, well, let's take the words that we agree on and then I'll focus on what we don't agree on. These are from Yehuda's recent papers.
Vitamin D affects the immune system at many levels and by a number of mechanisms .. Vitamin D has multiple immunosuppressant properties .. On the whole, vitamin D confers an immunosuppressive effect.2)
The possible involvement of vitamin D deficiency in the development of autoimmune diseases has recently gained interest .. the impact of the vitamin D pathway on immune function .. its influence on both autoimmune diseases and cancer should be further elucidated. 3)
I agree with that 100%. There is just one word on that page which I believe is totally incorrect. And that is the word “deficiency”. In this presentation I am going to explain how the vitamin D metabolism in man really works and why the concept of deficiency is incorrect.
#2 What is a VDR?
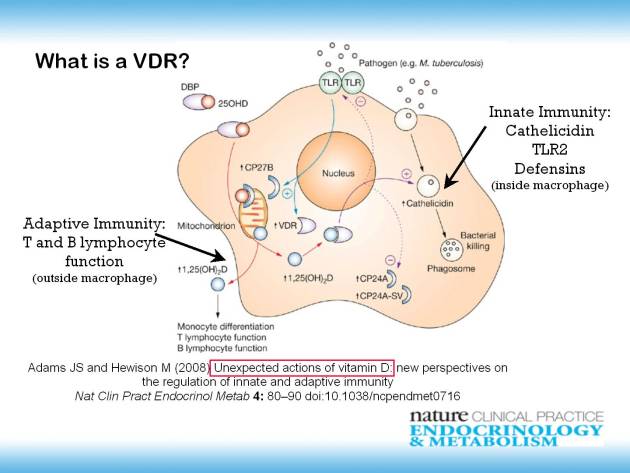
Vitamin D is important because it's associated with a nuclear receptor called the VDR. The VDR is a nuclear receptor which is diagrammatically shown here as just one element inside a cell. You have a macrophage. Here a nucleus cytoplasm. All of the things going on in the cytoplasm. If you want more details you can look on Wikipedia, or you can look in Nature Clinical Practice at this citation here.4)
The VDR is important both for adaptive immunity, the T and B lymphocyte function outside the macrophage. And it's particularly important for innate immunityThe body's first line of defense against intracellular and other pathogens. According to the Marshall Pathogenesis the innate immune system becomes disabled as patients develop chronic disease.. It transcribes cathelicidin, TLR2, and the defensins inside the macrophages. The main defenses that our phagocytes have against pathogens getting inside the immune system.
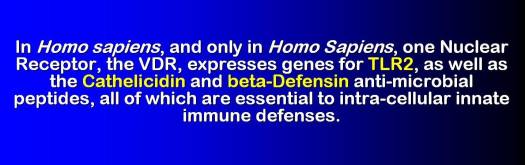
#3 Innate Immune VDR functions are unique to Homo Sapiens
The important thing is that the innate immune functions of the VDR are unique to Homo sapiens. In Homo sapiens, and only in Homo sapiens, there is one nuclear receptor, the VDR, which expresses genes for TLR2, as well as the cathelicidin and beta-defensin An antimicrobial peptide found primarily in immune cells and transcribed by the Vitamin D Receptor. anti-microbial peptides, all of these are essential to the intracellular innate immune defenses.
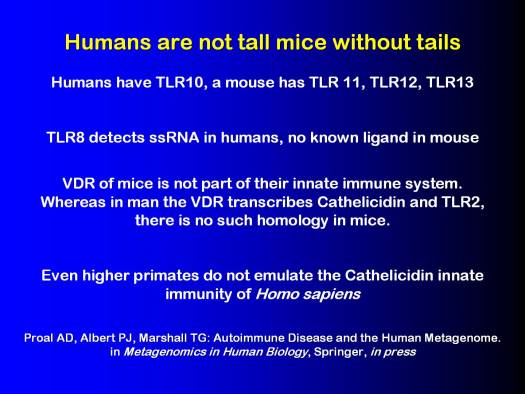
#4 Humans are not tall mice without tails
Humans are not tall mice without tails. They have different numbers of Toll-Like Receptors, for example. Humans have Toll-Like Receptor 10 and a mouse has Toll-Like Receptors 11, 12, and 13. In humans TLR8 detects single strand RNA, while TLR8 in the mouse, we don't know what it does yet. The VDR of mice is not part of their innate immune system.
You cannot study the vitamin D receptorA nuclear receptor located throughout the body that plays a key role in the innate immune response. in mice, how it relates to the immune system, and expect it to translate to Homo sapiens. It doesn't work.
Whereas in man the VDR transcribes cathelicidin, which is the primary anti-microbial which produces peptides that protect the phagocytes themselves. And TLR2, which is the primary toll-like receptor which detects pathogens inside the macrophages, there is no such homology in mice.
In mice, there are other receptors, there are other genes that do that. Even the higher primates do not emulate the cathelicidin innate immunity of Homo sapiens.
For more information, we have just written a chapter, Autoimmune Disease and the Human Metagenome in the textbook, Metagenomics in Human Biology. That is coming out next month.
#5 Homo sapiens VDR, Olmesartan in LBP
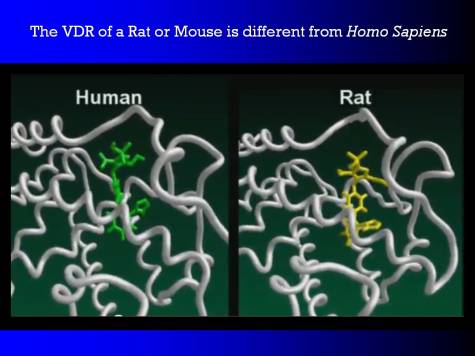
Here we have molecular dynamics of the VDR receptor of Homo sapiens. And there is a drug sitting in the binding pocket. This drug is olmesartan. The activated vitamin D itself sits in about the same spot. The green molecule is olmesartan.
Now if we look at the VDR of Rattus norvegicus, the VDR looks basically the same. But there are a number of amino acids that are different. And in particular, the amino acids that bind to that tetrazole moiety in human beings, here on the left, do not exist in the rat.
Here [in the VDR of the rat] you can see the tetrazole is wandering around aimlessly instead of having the two hydrogen bonds that cause it to be an agonist in Homo sapiens. In the rat, this particular drug has no similar effect.
You have got to be very, very careful when using animal models in the VDR, because the VDR is a highly evolved mechanism.
#6 The NIH Human Microbiome Project
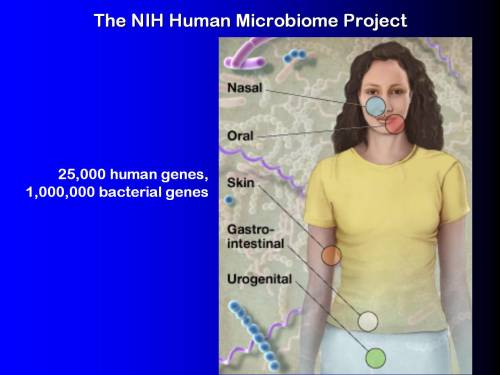
Well, the NIH Human MicrobiomeThe bacterial community in the human body. Many species in the microbiota contribute to the development of chronic disease. Project has been trying to identify how many genes, and in particular just how many genes coming from microbiotaThe bacterial community which causes chronic diseases - one which almost certainly includes multiple species and bacterial forms., bacterial and viral genes exist in the human body. The estimate is about 25,000 human genes and about a million bacterial genes.
Where do they exist? Well, some of them are in all the normal places. We saw them on the previous shot. The nasal, oral, skin, GI cavities, etc. The places we expect to find bacteria. But there are also bacteria inside the immune system, persistent infections.
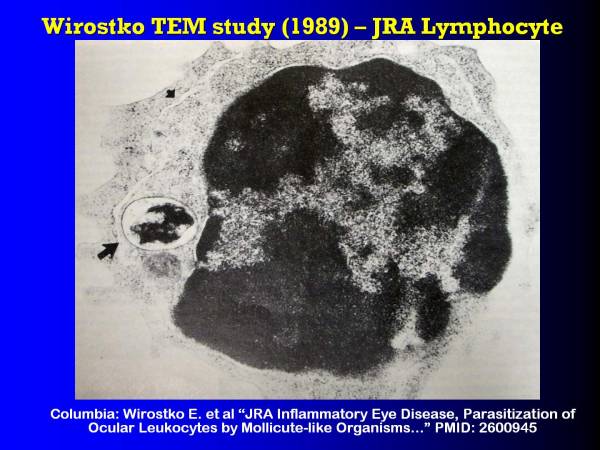
#7 Wirostko TEM Study-JRA Lymphocyte
This is a transmissionAn incident in which an infectious disease is transmitted. electron microscope photograph from 1989, Columbia University, done by Emil Wirostko's group and he has stained in Juvenile Rheumatoid Arthritis lymphocyte (but it's also in the macrophages and monocytes, as well as the lymphocytes).
There are regions of bacteria DNA which are stained with uranyl-acetate. There are these long, thin, extruded, ah, I guess I could call them biofilms A structured community of microorganisms encapsulated within a self-developed protective matrix and living together. [upper left smaller arrow]. They are only biofilms in that they are an extruded bacterial protein. Then there is this big colony here [lower left arrow], living in the cytoplasm of this lymphocyte.
This is the nucleus of the lymphocyte [darker central area]. The nucleus is somewhat under stress as you can see.
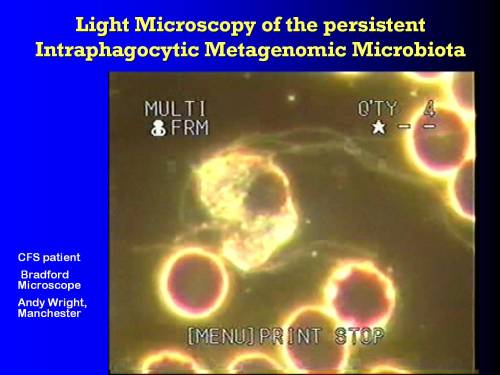
#8 Light microscopy of the persistent intraphagocytic metagenomic microbiota
When we look at them with light microscopy, then what we can see… this is a monocyte which has just started to explode from the pressure of the pathogens in it's cytoplasm.
You see it's nucleus is still intact. Throwing out these long, thin filaments. Filaments which come from bacterial proteins.
There's no homologue that produces that type of filament in man.
#9 Salivary microbiome
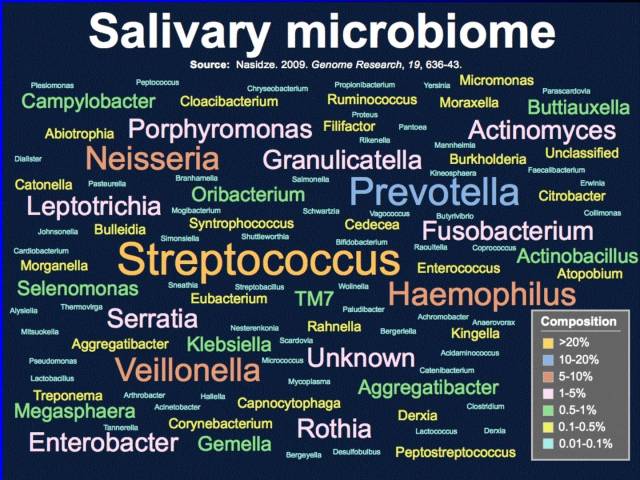
If we look at even simple genomes, if we look at the microbiome of the mouth, the salivary microbiome. We are talking about hundreds, literally 500 plus species of bacteria that have already been identified in the saliva of healthy individuals.
This study was done by Max Planck.5) It was done on a number of healthy individuals all over the world. There was more variation between individual and individual than there was from country to country. In particular, look at these [highlighting items in chart], Yersinia (the plague), Porphyromonas, Neisseria, Streptococcus. (The size of the text is approximately relative to concentrations that were found.) A whole series of species that one would never to expect to find in healthy saliva, but it's there.
And you can only see it when you use molecular technologies, when you sequence the RNA that you find in the mouth and you match it up with the known genomes, of known bacterial species (they are not all pathogens).
#10 Hip Joint Microbiome
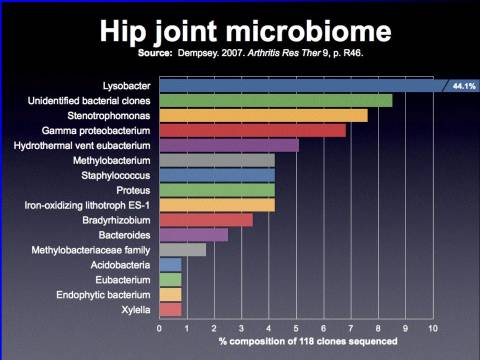
In a hip joint, this was a study done by Dempsey in 2007, and not surprisingly a large number of the species were typical biofilm A structured community of microorganisms encapsulated within a self-developed protective matrix and living together. type species Lysobacter is a gliding bacterium. Also, Staphylococcus is another non-biofilm formation.
But look at this here, hydrothermal-vent Eu bacterium. Something which is not supposed to be in the human body, and certainly is not going to be a contaminant in a clean surgical environment, was sequenced using DNA technology, or RNA technology, out of the removed hip joints during hip revision arthroplasty.
#11 Accumulated metagenome determines the clinical disease symptomatology
Many, many human metabolites are affected by the metagenome, and the sum total of all the interactions between each genome, each pathogenic genome and the human genome, gives rise to the totality of symptoms suffered during chronic disease.
The genes from bug “A”, plus the genes from bug “B” create the environment for disease “X” to manifest. And, as another example, genes from bugs “C”, “D”, “E”, “F”, and without bug “G”, because many of those species are pathogenic to each other, could very well lead to the disease “Y”.
So now we are beyond the postulates of Koch where one bacterium, or one species, leads to one disease. Now that we understand at the level of individual proteins, individual enzymes, how the species are starting to interact, we can see that we have a really difficult problem to solve.
The genomes accumulate gradually during life, incrementally shutting down the innate immune system. Genes from the accumulated metagenome determine the clinical disease symptomatology. And in many people they don't end up with a diagnosable disease, they just end up with the aches and pains of the aging, maybe with a cardiovascular terminal event, or maybe something like dementia.
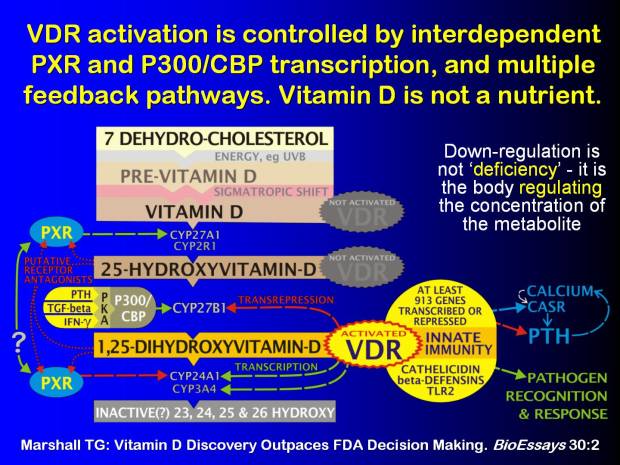
#12 Vitamin D is not a nutrient
I said that vitamin D deficiency is a flawed concept. The reason it is a flawed concept is because vitamin D is not a nutrient. A vitamin is defined as something that the body does not make. We've known for decades that the body makes it's own vitamin D. And it doesn't need sunshine to do it either. It makes the vitamin D within the cells that need vitamin D from a substrate, 7-dehydro-cholesterol, via a number of other transcription factors.
There is PXR, which is another nuclear receptor. And then there's P300/CBP, which is another transcription factor. Creating enzymes that take the 7-dehydro-cholesterol through a 25-hydroxy-vitamin-d stage (which is an intermediate that most of you would be measuring in your patients) to the activated form 1,25-dihydroxy, which then activates the VDR and allows the innate immunity to go forward.
But there are feedback paths. Feedback paths from the activated VDR. Feedback paths into the PXR as well. There are feedback paths. There are feed forward paths. This is a tightly controlled steroid. It is not a first-order mass-action vitamin. It's a controlled steroid. There's more information in my paper, “Vitamin D Discovery Outpaces FDA Decision Making.”6)
The important thing to know is down-regulation is not 'deficiency'- it is the body regulating the concentration of the metabolite. When you observe a lowered level of this metabolite in the body [highlighting 25-hydroxy-vitamin-d], it is because the body is trying to regulate it down. To make the metabolism work better.
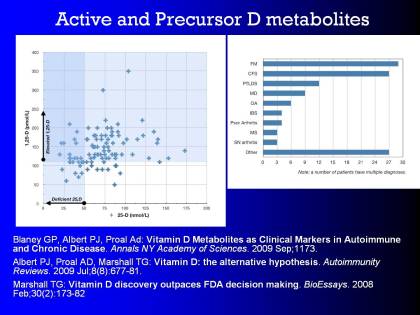
#13 Active and Precursor D metabolites
I won't go into active and precursor D metabolites.
My colleague, Dr. Blaney has written on that, and he, I'm sure, will go into that in the subsequent presentation. But here are some citations if you are interested.
Blaney GP, Albert PJ, Proal AD: Vitamin D Metabolites as Clinical Markers in AutoimmuneA condition or disease thought to arise from an overactive immune response of the body against substances and tissues normally present in the body and Chronic Disease. Annals NY Academy of Sciences. 2009 Sep;1179.
Albert PJ, Proal AD, Marshall TG: Vitamin D: the alternative hypothesis. Autoimmunity Reviews. 2009 Jul;8(8):677-81.
Marshall TG: Vitamin D discovery outpaces FDA decision making. BioEssays. 2008 Feb;30(2):173-82
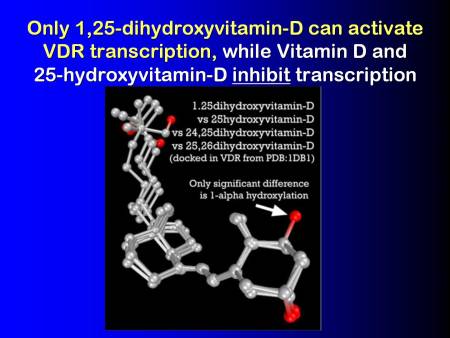
#14 Only 1,25-dihydroxyvitamin-D can activate VDR transcription
The important thing to note is that the vitamin D and the 25-hydroxyvitamin-dThe vitamin D metabolite widely (and erroneously) considered best indicator of vitamin D "deficiency." Inactivates the Vitamin D Nuclear Receptor. Produced by hydroxylation of vitamin D3 in the liver. precursors, that you normally use clinically, actually inhibit transcription by the VDR. They actually are immunosuppressive. I agree 100% with Yehuda and his colleagues. Vitamin D, exogenous vitamin D, is immunosuppressive.
And, only the 1,25-dihydroxyvitamin-d, or calcitriol, can actually activate VDR. And it can only do it in a paracrine fashion, within the cells.
1,25-dihydroxyvitamin-D vs 25-dihydroxyvitamin-D
vs 24,25-dihydroxyvitamin-D vs 25,26-dihydroxyvitamin-D
(docked in VDR from PDB:1DB1)Only significant difference is 1-alpha hydroxylation
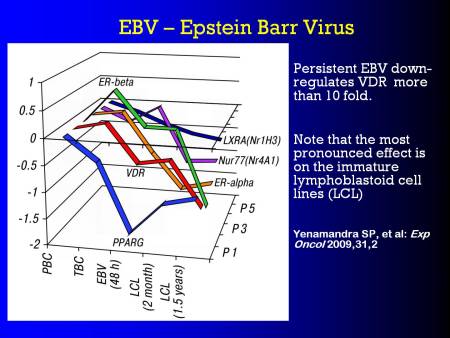
#15 EBV - Epstein-Barr Virus
Well, look, if you were a pathogen, and you wanted to persist in a patient, it would make sense that you would want to knock out the defenses of the cells that you were living within.
EBV is an obligate pathogen. We know that it lives within the cytoplasms of the phagocytes. EBV knocks out VDR. By knocking out VDR, it allows itself to persist, because it stops the body from producing it's anti-microbials, it's endogenous anti-microbials, and the TLR2, which is a key part of the defense recognition mechanism. EBV does that. And in particular, in the lymphoblastoid cell lines (LCL), the 18 month cell lines and the 2 month cell lines, the VDR is down-regulated progressively as time goes by.
Persistent EBV down-regulates VDR more than 10 fold.
Yenamandra SP, et al: Exp Oncol 2009,31,2
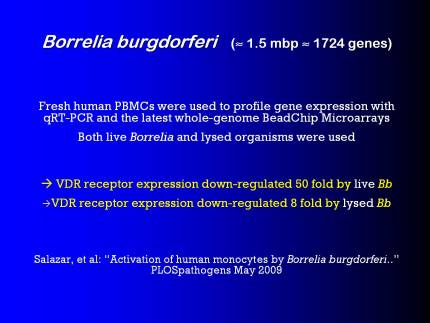
#16 Borrelia burgdorferi
Another pathogen that knocks down VDR very effectively is Borrelia burgdorferi. That down regulates VDR expression 50-fold with live spirochetes, and about 8-fold with the lysed for of Borrelia.
Fresh human PBMCs were used to profile gene expression with qRT-PCR and the latest whole-genome BeadChip Microarrays
Both live Borrelia and lysed organisms were used
→ VDR receptor expressions down regulated 50 fold by live Bb
→ VDR receptor expressions down regulated 8 fold by lysed BbSalazar, et al: “Activation of human monocytes by Borrelia burgdorferi…” PLOSpathogens May 2009
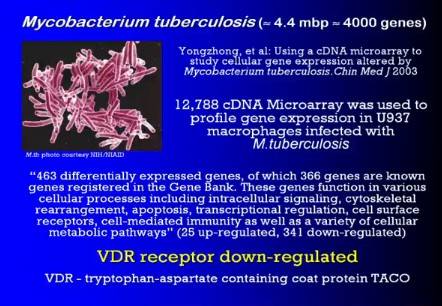
#17 Mycobacterium tuberculosis
And of course, the bacterium that Yehuda identified back in the 1970's as being at the heart of autoimmunity in some way, in his early papers, Mycobacterium tuberculosis.
The way that this pathogen evades the immune system and can live within the phagocytes, is it down-regulates the expression of the VDR nuclear receptor. It down-regulates the ability of the phagocytes to fight it.
Yongzhong, et al:Using a cDNA microarray to study cellular gene expression altered by Mycobacterium tuberculosis. Chin Med J 2003
12,788 cDNA Microarray was used to profile gene expression in U937 macrophages infected with M. tuberculosis
“463 differentially expressed genes, of which 366 genes are known genes registered in the Gene Bank. These genes function in various cellular processes including intracellular signaling, cytoskeletal rearrangement, apoptosis, transcriptional regulation, cell surface receptors cell-mediated immunity as well as a variety of cellular metabolic pathways”
(25 up-regulated, 341 down-regulated)VDR receptor down-regulated
VDR - tryptophan-aspartate containing coat protein TACO
#18 Vitamin-D 'deficiency' in Tuberculosis
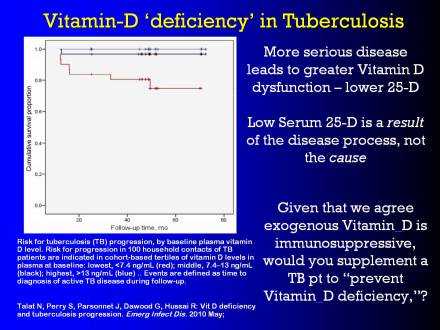
So, let's have a look at this paper that's just come out, last week actually, in Emerging Infectious Diseases, a CDC publication. And it showed vitamin-D 'deficiency' in tuberculosis.
What it showed was that the mortality from tuberculosis increased, the mortality increased, as the level of 25-DThe vitamin D metabolite widely (and erroneously) considered best indicator of vitamin D "deficiency." Inactivates the Vitamin D Nuclear Receptor. Produced by hydroxylation of vitamin D3 in the liver., the vitamin-D precursor in the blood stream decreased.
So if the body is not down-regulating the 25-D, then patients have a far better life expectancy, a lower chance of morbidity from tuberculosis than if they have a low level of 25-D.
Graph: cumulative survival proportion over time
Talat N, et al: Vitamin D deficiency and tuberculosis progression. Emerg Infect Dis. 2010 May
Well, that's fair enough, but the thing is, if we talk about this as a deficiency, then the temptation is to say, “well, let's intervene… let's give the person some of this vitamin D to replace this 'deficiency.'” But as we agreed on that first slide with Yehuda, vitamin-D, exogenous vitamin-D, is immunosuppressive. We all agree with that, whether it's molecular biology, or clinical medicine.
So, would we give exogenous vitamin-D, which we know is immunosuppressive to try and prevent TB from becoming a morbid condition? Well, I wouldn't. We have to remember that low serum 25-D is a result of the disease process, and not the cause. The more serious the disease, the greater the mortality, the greater the vitamin-D dysfunction, and the lower the measured 25-D quartile.
#19 Infection and Autoimmunity
We all agree that infection is somehow related to autoimmunity. We've had whole conferences here on autoimmunity, in Budapest, and subsequent to that. So if we wouldn't give it in tuberculosis, why are we considering that vitamin D supplementation might be useful in autoimmunity, where there's also likely an infective component?
So, what we did, once we understood exactly how the vitamin D metabolism was working, we chose immunostimulation or immunosuppression.
We found a drug, which happened to activate the vitamin D [receptor]. It is a perfectly safe ARBA drug which is an angiotensin receptor blocker. One of the ARBs is olmesartan (Benicar). Not all ARBs activate the Vitamin D Receptor.. When you change the dosing of it, it has a good action on the VDR and it starts the innate immune system working again. To the extent that people normally taking large doses of antibiotics, the moment they take the VDR agonist, they become very sensitive to even small doses of antibiotics. It's immune stimulation, rather than immunosuppression.
#20 Response to Immunostimulatory Treatment
This is data that [Capt. Tom Perez] presented at Porto, showing a whole range of autoimmune conditions, and the positive responses that we have been achieving using immunostimulation, rather than immunosuppression over the last eight years.
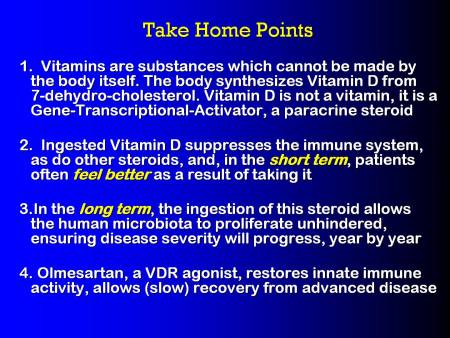
#21 Take Home Points
1. Vitamins are substances which cannot be made by the body itself. The body synthesizes vitamin D from 7-dehydro-cholesterol. Vitamin D is not a vitamin, it is a Gene-Transcriptional-Activator, a paracrine steroid.
2. Ingested Vitamin D suppresses the immune system, as do other steroids, and, in the short term, patients often feel better as a result of taking it.
3. In the long term, the ingestion of this steroid allows the human microbiotaThe bacterial community in the human body. Many species in the microbiota contribute to the development of chronic disease. to proliferate unhindered, ensuring disease severity will progress, year by year.
4. Olmesartan, a VDR agonist, restores innate immune activity, allows (slow) recovery from advanced disease.
That's all. Thank you very much.
#22
#23
[PMID: 17557889] [PMCID: 1955167] [DOI: 10.1136/ard.2007.069831]
[PMID: 18212810] [PMCID: 2678245] [DOI: 10.1038/ncpendmet0716]