Related article: Non-MP antibacterials

Table of Contents
Urinary symptoms
Acute infections commonly cause a range of unpleasant urinary diseases and symptoms including cystitis. Chronic infections also cause diseases such as interstitial cystitis, kidney stones, and hematuria.
Sometimes a urinary symptom masks as an infection and is actually immunopathologyA temporary increase in disease symptoms experienced by Marshall Protocol patients that results from the release of cytokines and endotoxins as disease-causing bacteria are killed.. Adjusting the Marshall ProtocolA curative medical treatment for chronic inflammatory disease. Based on the Marshall Pathogenesis. (MP) medications is the best way to manage symptoms of immunopathology.
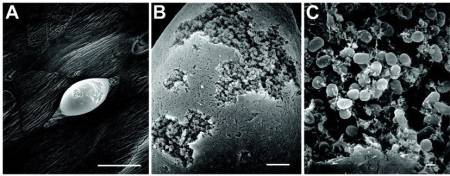
Urine is not sterile
While urine within the urinary tract has been traditionally regarded as “sterile”, this assumption relies on culture-based methods, which capture a small fraction of microbial richness. A 2011 pyrosequencing study looked at 16S rDNA amplicons of eight culture-negative healthy female urine specimens.1) The study found significant diversity, with the predominant genera detected being Lactobacillus, Prevotella and Gardnerella. Notably, a significant amount of sequences belonging to bacteria with a known pathogenic potential was observed.
Urinary tract infection (UTI)
The medical term for bladder or urinary tract infection (UTI) is cystitis, which literally means inflammationThe complex biological response of vascular tissues to harmful stimuli such as pathogens or damaged cells. It is a protective attempt by the organism to remove the injurious stimuli as well as initiate the healing process for the tissue. of the urinary bladder. A UTI is often caused by an acute bacterial infection. UTIs can occur in any part of the urinary tract including the kidneys, ureters, urethra and bladder. UTIs are more common in women because a woman's shorter urethra provides easier access for bacteria, but men are also susceptible.
Symptoms of a UTI include:
- urgent desire to empty the bladder
- frequent urination
- burning or pain during urination (dysuria)
- bladder spasms
- the feeling of having to urinate even though little or no urine actually comes out
- in some cases, a cloudy, bloody or foul-smelling urine
- in some cases, a mild fever
A UTI is diagnosed with a urinalysis to assess the amount of bacteria in the urine. Although urine contains a variety of fluids. salts, and waste products, it normally does not have bacteria in it. Sometimes a culture of the bacteria is done to determine the appropriate antibiotic. Until one's doctor does a culture and sensitivity, any antibiotic a patient is given for a urinary tract infection is an educated guess.
Irritation in the urinary tract is not related to the alkalinity or acidity of urine.
If the urinalysis is positive
If a urinalysis is positive for bacteria and one's doctor wants to use an antibiotic other than minocycline, ask him or her to consider Ceftin, Biaxin or a fluoroquinolone, which will not interfere with immunopathology.
Other strategies for managing a UTI include:
- Standard measures for managing immunopathology – Try slowing the immune system reaction to see if symptoms of cystitis are relieved.
- Cranberries and cranberry drinks/supplements – A substance in cranberries may help clear bacteria from the urinary tract by preventing bacteria from sticking to mucosal surfaces lining the bladder and gut.2) The recommended dosing for prophylaxis of urinary tract infection is based on a recent positive randomized controlled trial that used one tablet of concentrated cranberry extract (300 to 400 mg) twice daily, or 8 oz of pure unsweetened cranberry juice three times daily. Note that pure unsweetened cranberry juice can be added to clear diet soda (e.g. Diet 7-Up) to make a more palatable drink. To be effective in preventing UTIs, cranberry must be taken without interruption in order to maintain its physical presence in the bladder.
- Avoid consumption of sugars especially D-mannose. Sugars contribute to the growth of pathogenic bacteria.
If the urinalysis is negative
- Symptoms of UTI may be due to immunopathology – The release of endotoxins and cytokineAny of various protein molecules secreted by cells of the immune system that serve to regulate the immune system. storm that follows bacterial die-off can mimic symptoms of cystitis. Marshall Protocol patients with cystitis whose urinalysis does not reveal a bladder infection may be experiencing immunopathology. Genital irritation may be due to vulvodynia. This may or not be related to an alteration in the pH of urine. If this is the case, a medical exam is suggested.
- Symptoms of UTI may be due to a subclinical infection – One study found that a large fraction of fastidious and anaerobic bacteria (22.43%) was not detected under culture conditions but only by using PCR, a genomic sequencing technique which is more rigorous at identifying bacteria.3) If this is the case the MP is still a patient's best option for ridding him or herself of the conditions which originally caused this problem.
Note that excessive urination, known as polyuria, may be due to subclinical kidney inflammation.
Kidney stones
Main article: Kidney stones
Related article: Flank pain
Kidney stones, also called renal calculi, are crystal aggregations of dissolved minerals in urine. Kidney stones typically form inside the kidneys or bladder and can primarily consist of a variety of substances including calcium oxalate, uric acid, and struvite (magnesium, ammonium and phosphate). According to the Marshall PathogenesisA description for how chronic inflammatory diseases originate and develop., there are two factors that seem to play a role in kidney stone formation: elevated levels of 1,25-DPrimary biologically active vitamin D hormone. Activates the vitamin D nuclear receptor. Produced by hydroxylation of 25-D. Also known as 1,25-dihydroxycholecalciferol, 1,25-hydroxyvitamin D and calcitirol. and the presence of bacteria.
Patients on the Marshall Protocol (MP) are somewhat less likely to get kidney stones, especially in later stages of the treatment, due to the restoration of proper vitamin D metabolism. Those patients who do develop kidney stones since starting the MP, should know they are a result of months or years of development and not due to the effects of the MP. The MP should prevent recurrence.
Interstitial cystitis/painful bladder syndrome
Interstitial cystitis/painful bladder syndrome is a urinary bladder disease of unknown cause characterized by pain associated with urination (dysuria), urinary frequency (as often as every 10 minutes), urgency, and pressure in the bladder and/or pelvis.
Patients experiences
My interstitial cystitis has improved greatly on the MP. Before the MP, I went for eight years in need of five medications everyday and no relief. I did not respond to Ciprofloxacin and showed no bacteria according to the urologist. I wanted to kill myself as it was so bad. After eight months on MP, I do not need any more meds, and the interstitial cystitis is doable. Before the MP, there were no antibiotics to treat IC as they considered it an inflammatory disease.
Lori, MarshallProtocol.com
Bacterial vaginosis
Bacterial vaginosis is a common syndrome associated with numerous adverse health outcomes in women. According to a 2012 study using broad-range PCR , the community of vaginal bacteria detected in subjects with BV was much more taxon rich and diverse than in subjects without BV.4) Actinobacteria and Bacteroidetes were strongly associated with BV.
Hematuria
Hematuria, or haematuria, is the presence of red blood cells (erythrocytes) in the urine. It can be a sign that there is a kidney stone or a tumor in the urinary tract (kidneys, ureters, urinary bladder, prostate, and urethra), ranging from trivial to lethal. If white blood cells are found in addition to red blood cells, then it is a signal of urinary tract infection.
Patients experiences
I had haematuria also and because I was hypercalcaemic, had calcium oxalate kidney stones…. Since going on the MP, I don't have anymore stones forming or passing and my haematuria has gone.
Simom Elrahi, MarshallProtocol.com
[PMID: 22047020] [PMCID: 3228714] [DOI: 10.1186/1471-2180-11-244]
[PMID: 17694340] [DOI: 10.1007/s10096-007-0379-0]
[PMID: 18336452] [DOI: 10.1111/j.1439-0272.2007.00830.x]
[PMID: 18487399] [PMCID: 2519371] [DOI: 10.1128/AEM.02884-07]


