Main article: High-dose antibiotic therapies

This is an old revision of the document!
Table of Contents
Chronic Lyme disease
Acute Lyme disease is widely recognized by the medical community, but there is a great deal of debate over the existence of chronic Lyme, also known as post-treatment Lyme disease syndrome. Some researchers have suggested that chronic Lyme does not exist. This may be because patients who are treated with high-dose antibiotics for Lyme do not recover. Generally speaking, mainstream medicine assumes that if an infectious agent causes a disease, a patient should be at least cured, if not helped, by an antibiotic. Therefore, the very existence of the disease is questioned. The fact that many so-called chronic Lyme patients test negative for Borrelia does not help either.
Many who acknowledge its existence have argued that chronic Lyme disease is caused by a single pathogen, Borrelia. But, according to the Marshall PathogenesisA description for how chronic inflammatory diseases originate and develop., the condition is caused by a community of microbes, one of which includes Borrelia. Borrelia is one of an increasing number of microbes documented to slow activity of the Vitamin D ReceptorA nuclear receptor located throughout the body that plays a key role in the innate immune response., undoubtedly in order to gain a survival advantage. It is for this reason that merely targeting Borrelia is not sufficient to recover from Lyme. In order to recover, patients sick with chronic Lyme need to activate the immune response to target a range of pathogens.
Clearly chronic Lyme patients are sick (and not with a mental condition), but this does not necessarily support the use of high-dose antibiotics, particularly since the drugs are demonstrably ineffective. Not unlike corticosteroidsA first-line treatment for a number of diseases. Corticosteroids work by slowing the innate immune response. This provides some patients with temporary symptom palliation but exacerbates the disease over the long-term by allowing chronic pathogens to proliferate., high-dose antibiotics are highly immunosuppressive, doing nothing to attack the pathogens responsible for chronic disease. Such drugs are merely causing an anti-inflammatory rather than an antibacterial reaction.
The Marshall ProtocolA curative medical treatment for chronic inflammatory disease. Based on the Marshall Pathogenesis. is an attempt to do the opposite. Rather than use immunosuppression, the MP uses antibiotics but at pulsed low doses in a way that minimizes immunosuppression. Further, antibiotics are optional. The main medication used by the MP is olmesartanMedication taken regularly by patients on the Marshall Protocol for its ability to activate the Vitamin D Receptor. Also known by the trade name Benicar. , which has antimicrobial properties.
Autoimmunity Research FoundationNon-profit foundation dedicated to exploring a pathogenesis and therapy for chronic disease. has been granted by the FDA orphan drug status for clindamycin in the treatment of post-treatment Lyme disease syndrome.
Managing symptoms while on the Marshall Protocol
- Pain – MP patients should always use 40mg of olmesartan (Benicar)Medication taken regularly by patients on the Marshall Protocol for its ability to activate the Vitamin D Receptor. every four hours before resorting to pain medications. However, when the usual strategies for managing immunopathology are not enough to control pain, MP patients rely upon pain medications. Except for corticosteroids, there is no pain medication contraindicated specifically because a patient is on the Marshall Protocol. Opioids are the preferred method of dealing with extreme pain in the MP cohort. See article Pain medication and muscle relaxants.
- Fatigue – The systematic use of stimulants to manage symptoms of fatigue is not recommended.
- Insomnia and poor sleep – The inability to sleep or sleep deeply is a common symptom of chronic inflammatory disease and can be exacerbated during periods of immunopathologyA temporary increase in disease symptoms experienced by Marshall Protocol patients that results from the release of cytokines and endotoxins as disease-causing bacteria are killed.. Restful sleep can help a patient to cope with other symptoms. It is not necessary to get all one's restful sleep at night. In fact, if a patient can, sleeping during the day may give him or her enough energy to accomplish any responsibilities for the day. See article, Sleep medications.
- Cognitive dysfunction – Cognitive dysfunctionThe loss of intellectual functions such as reasoning; memory loss; and other neurological abilities that is severe enough to interfere with daily functioning. (also known as brain fogThe loss of intellectual functions such as reasoning; memory loss; and other neurological abilities that is severe enough to interfere with daily functioning.) is the loss of intellectual functions such as thinking, remembering, and reasoning of sufficient severity to interfere with daily functioning. Patients with cognitive dysfunction have trouble with verbal recall, basic arithmetic, and concentration.
- Physical activity and exercise – The choice to exert oneself through physical activity or exercise should be made in the light of the stage of one's disease and the effect that extra activity has on the immune system. In different patients under different circumstances, exercise is capable of either suppressing or increasing the immune response. MP patients who can perform their activities of daily living while recovering on the MP are as fit as they need to be. Their focus should be in regaining their health with the MP. With improved health will come improved ability to exercise and increase endurance.
Statistics
from DJ in California During the summer of 2013 I looked at 2,000 records of people using the Marshall Protocol.
I eliminated all records that had less than 20 messages, as these were usually inquiries into the treatment without actual participation. I eliminated all records from people who had been banned from the site. I eliminated all records from Health Professionals who did not actually have disease. I eliminated all records where I could not find a valid progress report. This left me with 864 meaningful records.
I tried my best to be unbiased as I was expecting to see about a 20% improvement in health of members, or in other words a 20-25% success rate. I was intending to compare this to the 10% success rate I found done on the use of prednisone to treat Sarcoidosis. That double blind report shows that 10% treated with prednisone achieve remission. (BTW remission in Sarcoidosis as far as I can find out is measured rather subjectively)
The following information is what I found:
Chronic Fatigue Syndrome: 183 members; 110 success; 30 no success; 43 unsure
Other Th1 diseasesThe chronic inflammatory diseases caused by bacterial pathogens.: 184 members; 110 success; 30 no success 44 unsure
TOTALS: 864 members;573 report success; 119 report no success; and for 172 results are not clear. SUCCESS RATES: Over all success rate 66.32% Over all unsuccessful 13.77% Over all unsure 19.91%
Lyme disease success 66.9%
All Other Th1 diseaseAny of the chronic inflammatory diseases caused by bacterial pathogens. success 59.8%
What we who are a part of this forum, who stuck with the protocol long enough, who endured the IP and were able to keep a doctor, report is that this has a better than 50% success rate.
Antibiotic treatments
One of the reasons why chronic Lyme disease is so contentious is that advocates for it strongly believe in the value of high-dose antibiotic therapies, any treatment which uses antibiotics at a large enough dose that the immune response is suppressed more than it is not. High-dose antibiotics are ineffective, and this is well-reflected in the published literature. The short-term improvement and long-term crash some patients feel on high-dose antibiotics is due to the fact these drugs interfere with immune activity in dose dependent fashion. With a weakened inflammatory response, a patient's symptoms may temporarily improve, but not because the pathogenic bacteria which drive disease have been eradicated. As a result, these protocols do not generate sustained immunopathology.
Doxycycline
Main article: Doxycycline
Although the MP antibiotic minocycline is also a tetracycline, doxycycline and minocycline are significantly different from each other – both in terms of structure and function. Doxycycline's effectiveness over short periods of time is due in part to the relatively high doses at which it is typically administered: 200 mg per day. Doxycycline does not kill as wide a range of bacteria as minocycline. For example, doxycycline doesn't kill Staphylococcus, a genus found in at least three recent studies in which the human microbiomeThe bacterial community in the human body. Many species in the microbiota contribute to the development of chronic disease. was sequenced.
Cephlasporins including Rocephin
Main article: Beta-lactam antibiotics
Related article: High-dose antibiotics
Patients with Lyme disease are often given high doses of intravenous ceftriaxone (Rocephin) and without any indication that the treatment is effective – even in the short-term.1) In fact, Rocephin only contributes to disease over the long-term.
Fallon et al treated patients diagnosed with Lyme disease with intravenous ceftriaxone (Rocephin) for a period of 24 weeks.2) While patients in the experimental arm of the trial experienced improvement in pain, fatigue, and physical functioning, these changes were short-lived. According to Fallon:
The improvement… was not sustained to week 24…. 10 weeks of IV ceftriaxone followed by 14 weeks of no antibiotic is not an effective strategy.
B.A. Fallon, et al. 3)
The study also revealed that more than one quarter of antibiotic-treated patients had significant adverse effects necessitating treatment termination.
In a letter to the editor, one physician writes:
140 g of ceftriaxone should have eliminated any spirochetes present in these patients…. In sum, this is now the fourth randomized blinded trial of prolonged antimicrobial therapy in patients previously treated for Lyme disease. Like the other three, it clearly demonstrates the absence of any lasting improvement in cognitive function. Given the considerable risk of serious adverse events from prolonged [high-dose] antibiotic treatment, it is time to look elsewhere for an effective management strategy to help patients with persistent cognitive symptoms after treatment for Lyme disease. Clearly, enough is enough.
John J. Halperin MD 4)
Other controlled trials have found no improvement in treatment outcome when the length of the study was extended.5)
Other treatments
- colloidal silver – While colloidal silver is marketed for internal and external use as an alternative medical remedy, there is no scientific evidence of its effectiveness in vivoA type of scientific study that analyzes an organism in its natural living environment. for any medical condition. Also, it can permanently turn your skin silver.
- hydrogen peroxide – Delivered intravenously. The theory is that hydrogen peroxide releases extra oxygen inside the body, killing microbes. This dangerous therapy is based on an overly simplistic view of the body's metabolism. There are no large-scale studies proving hydrogen peroxide is effective.
- Rife – There is no scientific evidence that the use of a Rife device has the intended effect on infectious bacteria. Instead, most patients using Rife are likely administering themselves nothing more than an expensive placebo.
Role of infection
Caused by multiple microbes
Related articles: Koch's postulates, Successive infection and variability in disease
Lyme disease is considered to be caused by Borrelia species of bacteria but slowly evidence is accumulating which suggests that Lyme disease is a far more complex condition than Borreliosis alone. This hypothesis suggests that it may be more appropriate to regard Lyme disease as a tick borne disease complex. Over recent years numerous different microbes have been found in ticks which are known to be zoonotic and can coinfect the human host. The hypothesis suggests that multiple coinfections are invariably present in the clinical syndromes associated with Lyme disease and it is suggested that these act synergistically in complex ways.
D.C. Owen 6)
Since first being recognized as a disease in 1981, Lyme has been widely assumed to be caused by a single infectious agent: Borrelia. In fact, the very reason the diagnosis of chronic Lyme is so controversial is that blood tests of people with Lyme-like symptoms infrequently show ongoing Borrelia infection. The assumption that one and only species (or genus) of microbe could cause a given symptom presentation is the antiquated legacy of Koch's postulatesCentury-old criteria designed to establish a causal relationship between a causative microbe and a disease. Koch's belief that only one pathogen causes one disease has now been called into question as multiple postulates are increasingly considered out of date.. More recent research suggests that the symptoms of chronic Lyme are caused my many microbes.
W. Ian Lipkin's team sampled 286 adult ticks from the two counties in New York State where Lyme disease is endemic, looking for the prevalence of polymicrobial infection with Borrelia burgdorferi, Anaplasma phagocytophilum, Babesia microti, Borrelia miyamotoi, and Powassan virus.7) Seventy-one percent of the ticks harbored at least one organism; 30% had a polymicrobial infection. Infections with three microbes were detected in 5% of the ticks. One tick was infected with four organisms.
Australian ticks
Human Tick-Borne Diseases in Australia. 8)
Borrelia and the VDR
Related article: Metabolism of vitamin D and the Vitamin D Receptor
In the arms race of host–microbe co-evolution, successful microbial pathogens have evolved ingenious ways to evade host immune responses.9)
Studies have indicated that the dysregulation of VDRThe Vitamin D Receptor. A nuclear receptor located throughout the body that plays a key role in the innate immune response. may lead to exaggerated inflammatory responses, raising the possibility that defects in Vitamin D and VDR signaling transduction may be linked to bacterial infection and chronic inflammationThe complex biological response of vascular tissues to harmful stimuli such as pathogens or damaged cells. It is a protective attempt by the organism to remove the injurious stimuli as well as initiate the healing process for the tissue.. Further characterization of Vitamin D/VDR will help elucidate the pathogenesis of various human diseases and in the design of new approaches for prevention and treatment.
Jun Sun 10)
Since the VDR is at the heart of the innate immune system, bacteria can survive by discovering how to disable it through a variety of different actions. Actions accumulate and are more powerful than individual actions. In keeping with evolutionary theory, a growing number of substances and species have been shown to downregulate the activity of the VDR, one of which is Borrelia burgdorferi. Live Borrelia burgdorferi reduced VDR expression in monocytes (phagocytes) by 50 times, and lysates (“dead” Borrelia) reduced it by 8 times11)
Olmesartan is the main medication used by the Marshall Protocol and is believed to act as a VDR agonistA substance such as olmesartan (Benicar) or 1,25-D which activates the Vitamin D Receptor and transcribes the genes necessary for a proper innate immune response., counteracting Borrellia's effect on the Receptor and reversing the disease process.
Different proteins in cerebrospinal fluid
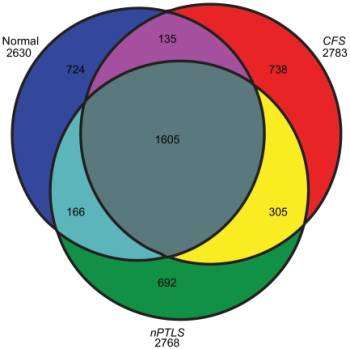
In a 2011 study appearing in PLoS One, Schutzer and colleagues analyzed spinal fluid samples from three groups — 11 healthy people, 43 diagnosed with chronic fatigue syndrome and 25 previously treated for Lyme disease but who were still experiencing cognitive problems and fatigue.12) Analysis of the fluid samples detected more than 2,600 proteins in each group. Most of the proteins appeared in all three groups. But 692 proteins turned up only in the Lyme patients and 738 others showed up only in the chronic fatigue group.
On its most basic level, this study offers strong evidence of a biological component for Lyme and CFS. The presence of so many unique proteins suggests that these are proteins are either created directly by microbes or are the results of microbes acting on the human genome.
In the aftermath of the study, several commentators have noted that this work could be built upon to more definitely distinguish Lyme from CFS. However, it is interesting to note that a significant number of proteins are common to both CFS and Lyme. The reductionist approach, in which a disease state is defined by a single or even a handful of proteins may not fully account for the complexity of human microbiomeThe bacterial community in the human body. Many species in the microbiota contribute to the development of chronic disease. and the nature of the disease process.
Autoantibodies
Greco et al. claimed to find a variety of autoantibodies including antiphospholipid antibodies in patients with chronic Lyme disease.13) Autoantibodies have long been tied to persistent infections.
Psychosomatic explanations for disease
Related article: Psychosomatic explanations for disease
Sigmund Freud and Jean-Martin Charcot were born 150 years ago, but their ideas about the effect of the subconscious on disease continue to resonate in the scientific community.14) Freud and colleagues argued that unconscious mental processes such as sublimated rage could manifest as physical symptoms. However, with the advent of superior technology, one by one, many diseases once supposed to be caused by psychological stress have since been attributed to other factors including infections.
According to the Marshall Pathogenesis, chronic fatigue syndrome, multiple chemical sensitivity and other chronic inflammatory diseases are likely caused by pathogens, yet many physicians consider these diseases to be “medically unexplained.” Medically unexplained diseases are widely prevalent15) but at the same time have few discernible markers or objectively measurable symptoms. While a lot of Freudian ideas have fallen out of favor, one legacy remains: difficult-to-explain diseases are still routinely attributed to psychological causes. The process by which patients supposedly manifest psychological problems as a disease has been named and renamed, classified and reclassified: hysteria, psychosomatic disorder, somatoform disorder, conversion disorder, functional disorder, etc. In each of these diagnoses, however, the stated origin of disease is unchanged: symptoms that cannot be explained are ultimately “all in a patient's head.”
While there is no denying the existence of some sort of “mind-body connection,” there is minimal compelling evidence that as the 19th century Swiss physician Georg W. Groddeck claimed: “Illness has a purpose; it has to resolve the conflict, to repress it, or to prevent what is already repressed from entering consciousness.”16) Despite the stark absence of evidence supporting these views, it is not unusual to read papers describing how patients with long-term so-called psychological illnesses may be subconsciously manifesting them, because it would allow them to have more “care, attention, disengagement, or even financial benefits.”17) Nor, is it uncommon for new theories to spring up along these lines. In one example, a 2008 continuing medical education publication taught physicians that when a celebrity becomes ill, healthy people are suggestible enough to develop long-term illnesses consistent with the celebrity's descriptions of their conditions. Such claims are recklessly speculative, harming patients and stalling needed research.
Treating patients who complain of so-called medically unexplained symptoms with cognitive behavioral therapy or, in the case of chronic fatigue syndrome, graded exercise therapy, may do more harm than good.18) The emergence of metagenomic technologies offers a more sophisticated set of tools for detecting and characterizing microbes in these disease states. Perhaps it is only the use of this technology that will finally relegate the notion of patient as attention-seeking victim to historical relic.
Herxheimer reaction
Related article: Immunopathology
Many members of the Lyme community are familiar with the notion of the Herxheimer reaction, the necessary increase in symptoms that occurs in the aftermath of an antibiotic treatment. The Herxheimer response, also known as herx, is roughly synonymous with immunopathology, the term more commonly used on this site and by patients on the Marshall Protocol.
One of the significant distinctions between a herx reaction in patients taking high-dose antibiotics and those on the MP is the length of that reaction. While it is common to hear Lyme patients experience a herx response for several weeks, patients on the MP may experience sustained immunopathology over the course of years. While this makes the MP harder to complete, the length of the treatment before a decrease in symptoms may be a tribute to how sick some patients with chronic Lyme or any other chronic disease truly are.
Ticks, what to do when bitten
Main article: Ticks, what to do when bitten
Marshall Protocol patients who develop a bulls-eye rash after a tick bite or who think a tick bite has put them at risk for Lyme disease should ask their physician about taking 100mg of minocycline twice daily for 30 days.
Chronic controversy over chronic Lyme disease
Lyme disease, with 20,000 cases reported annually, ranks low on the list of the most prevalent infectious diseases. But it ranks first in rancor generated in the medical community.
David Whelan wrote Ticks aren't the only parasites living off patients in borreliosis-prone areas
While there is general agreement on the optimal treatment for early Lyme disease, there is considerable controversy over the existence, prevalence, diagnostic criteria, and treatment of chronic Lyme disease.
Over the past decade, two opposing camps have emerged in the battle over Lyme. One camp is represented by the International Lyme and Associated Diseases Society (ILADS), which argues that Lyme disease is not rare because its spread is facilitated by rodents, deer and birds, and can be found in an unpredictable distribution around the world accompanied by other tick-borne coinfections that may complicate the clinical presentation. According to the ILADS, tick bites often go unnoticed and commercial laboratory testing for Lyme disease is inaccurate. Consequently, the disease is often not recognized and may persist in a large number of patients, requiring prolonged antibiotic therapy to eradicate persistent infection with the evasive Lyme spirochete.19)
The opposing camp is represented by the Infectious Diseases Society of America (IDSA), which maintains that Lyme disease is a rare illness localized to well-defined areas of the world. According to the IDSA, the disease is “hard to catch and easy to cure” because the infection is rarely encountered, easily diagnosed in its early stage by distinctive clinical features and in more advanced stages by accurate commercial laboratory tests, and effectively treated with a short course of antibiotics over 2-4 weeks. Chronic infection with the Lyme spirochete, Borrelia burgdorferi, is rare or nonexistent, and the concept of chronic Lyme disease rests on “faith-based” opinion rather than “evidence-based” science.20)
This mainstream view is exemplified by a 2007 review in the New England Journal of Medicine, which noted the diagnosis of chronic Lyme disease is used by a few physicians despite a lack of “reproducible or convincing scientific evidence”, leading the authors to describe this diagnosis as “the latest in a series of syndromes that have been postulated in an attempt to attribute medically unexplained symptoms to particular infections.”21)
Chronic Lyme disease is the most recent in a continuing series of “medically unexplained symptoms” syndromes. These syndromes, such as fibromyalgia, chronic fatigue syndrome, and multiple chemical sensitivity, meet the need for a societally and morally acceptable explanation for ill-defined symptoms in the absence of objective physical and laboratory findings. We describe factors involved in the psychopathogenesis of chronic Lyme disease and focus on the confusion and insecurity these patients feel, which gives rise to an inability to adequately formulate and articulate their health concerns and to deal adequately with their medical needs, a state of disorganization termed aporia.
L.H. Sigal 22)
Groups of patients, patient advocates, and the small number of physicians who support the concept of chronic Lyme disease have organized to lobby for recognition of this diagnosis, as well as to argue for insurance coverage of long-term antibiotic therapy, which most insurers deny, as it is at odds with the guidelines of the major medical organizations.
The term “Lyme-literate medical doctor” or LLMD has been coined to describe physicians who acknowledge the existence of chronic Lyme disease an infectious condition and are willing to treat it with antimicrobial therapies. LLMDs generally operate outside the mainstream of medicine. A number have been brought up before medical board reviews and been the subject of patient lawsuits.
The net result of this controversy is that many doctors try to avoid having Lyme patients in their practice.
Patient interviews
<html> <div class=“patientinterviews”>
<html>
<div class=“patientinterviewboxl”>
<div class=“patientinterviewimage”></html> <html></div>
<div class=“patientinterviewtext”>
<div class=“patientinterviewname”></html>Sue Andorn<html></div></html>
<html></div>
<div class=“patientinterviewtext”>
<div class=“patientinterviewname”></html>Sue Andorn<html></div></html>
Lyme, Babesia
Read the interview
<html></div></div>
<html>
<div class=“patientinterviewboxr”>
<div class=“patientinterviewimage”></html> <html></div>
<div class=“patientinterviewtext”>
<div class=“patientinterviewname”></html>Melinda Stiles<html></div></html>
<html></div>
<div class=“patientinterviewtext”>
<div class=“patientinterviewname”></html>Melinda Stiles<html></div></html>
Lyme disease, irritable bowel syndrome/ulcerative colitis, radiculitis
Read the interview
<html></div></div></html>
<html>
<div class=“patientinterviewboxl”>
<div class=“patientinterviewimage”></html> <html></div>
<div class=“patientinterviewtext”>
<div class=“patientinterviewname”></html>Ken L.<html></div></html>
<html></div>
<div class=“patientinterviewtext”>
<div class=“patientinterviewname”></html>Ken L.<html></div></html>
Post Treatment Lyme Disease Syndrome (PTLDS)
Read the interview
<html></div></div></html>
<html>
<div class=“patientinterviewboxr”>
<div class=“patientinterviewimage”></html> <html></div>
<div class=“patientinterviewtext”>
<div class=“patientinterviewname”></html>Robyn Russell (patient's mother)<html></div></html>
<html></div>
<div class=“patientinterviewtext”>
<div class=“patientinterviewname”></html>Robyn Russell (patient's mother)<html></div></html>
Lyme, myoclonus
Read the interview
<html></div></div></html>
<html>
<div class=“patientinterviewboxl”>
<div class=“patientinterviewimage”></html> <html></div>
<div class=“patientinterviewtext”>
<div class=“patientinterviewname”></html>P. Bear R.N.<html></div></html>
<html></div>
<div class=“patientinterviewtext”>
<div class=“patientinterviewname”></html>P. Bear R.N.<html></div></html>
chronic borreliosis (“Lyme”), multiple chemical sensitivities, chronic spinal inflammation, peripheral neuropathy
Read the interview
<html></div></div>
<br clear=“left” />
</div> </html> Interviews of patients with other diseases are also available.
Patients experiences
I am a late-stage Borrelia (Lyme) patient with co-infections. It was decades before I was properly diagnosed and treated. I have been around the block when it comes to treating Lyme and co-infections by the LLMD approved methods. I have done cholestyramine (Questran) with ABX treatment. As a matter of fact, I was one of the early Lyme pioneers with Dr. Shoe's neurotoxin therapy.
I recall that it took months for it to help me. Even then, the help was minimal - nothing compared to the MP. Actually, I was in my 3rd box before I noticed any improvement at all. Cholestyramine is not without its own side effects and risks, such as vitamin deficiency as a result of its ability to bind everything.
Prior to the MP, I was considered a treatment failure after 17 months of IV ABX followed by years of oral combinations that included a variety of ABX, flagyl, tinidazole, Mepron and diflucan. I can tell you, I wasted much time and vast amounts of money before I found the MP. This is the real deal and you don't really need to augment it with anything. Under no circumstances would I try combining it with cholestyramine. Based on my personal experience with both therapies used separately, it is not something I would ever be comfortable doing.
The MP is not a quick fix, but it really does work just as predicted. It is the only treatment that has ever handled all of my infections. (Lab confirmed: Borrelia, Babesia, Bartonella, mycoplasma, Candida, HHV-6 and EBV.) Prior to this protocol, I bought into the idea of a “carousel of tick-borne infections”, because it seemed that once I knocked one down, another popped up in its place. All of those positive tests and diagnoses I had bought into in the past are finally a thing of the past. These days, I am the proud owner of a fully functioning immune system and it is handling everything quite nicely.
At this point, I am in my 19th month on the protocol and I am in phase 3. I have been pretty remiss about posting progress because I am busy enjoying a level of health that I never before could have imagined. The MP meds and lifestyle have made this possible. Having been the LLMD route from 2000-2004, I can assure that they have nothing on TM and the MP. Unfortunately, it seems that our LLMDs are too lost in a quagmire of brain-fogged patients who are seeking quick fixes to recognize the full potential of this discovery.
Lonestartick
Read more
- According to a 2011 study, a Neolithic mummy had Borrelia, suggesting that Lyme disease has been around for quite some time.
- Chronic Lyme disease: A dubious diagnosis – A 2010 Chicago Tribune article portraying Lyme advocates as unscientific. This article well represents the view of many doctors concerning Lyme advocates.
- Chronic Lyme Disease and the "Axis of Evil" – A 2009 Future Microbiology paper written from the perspective of ILADS and LLMDs.
- SPECT scans are abnormal in chronic Lyme patients – According to a 2012 study, 75% of brain SPECT scans are abnormal in patients with chronic Lyme disease.23)
Notes and comments
broken link removed Lyme patients commiserate with one another over feeling worse after taking vitamin D.
Presentations and publications
Antibodies linked to long-term Lyme symptoms: Some patients with Lyme disease still show symptoms long after the… http://bit.ly/qbAFjv
From: Frenchie Date: 2011-08-09 07:08:55 Reply: http://www.marshallprotocol.com/reply.php?topic_id=13346
Now Armin Alaedini at Weill Cornell Medical College in New York and his colleagues have found that patients diagnosed with post-Lyme disease syndrome have antibodies that suggest they carried the infection for an unusually long time. The finding, published in Clinical Immunology1, might help the syndrome to be better understood, diagnosed and treated. Alaedini's team looked at antibodies made in response to a protein called VlsE, which is found on the surface of Borrelia burgdorferi, the tick-borne bacterium that causes Lyme disease. The antibodies recognize a snippet of the protein called an epitope, and recruit the immune system to attack the bacterium. The researchers found that post-Lyme sufferers have a greater variety of antibodies to this epitope than patients whose infection cleared up quickly. This finding suggests that patients with chronic symptoms have experienced a prolonged infection, caused by microbes that have evaded the immune system by varying the epitopes they carry. As a result of these variations, the body makes new antibodies targeting the modified protein. The longer the microbe manages to keep changing, the more diverse its host's antibodies become.
http://www.nature.com/news/2011/110805/full/news.2011.463.html#B1
From: Dr Trevor Marshall Date: 2011-08-09 07:16:27 Reply: http://www.marshallprotocol.com/reply.php?topic_id=13346
The group at Weill Cornell did not consider the possibility that their testing procedures might be confused by the thousands of other species present along with the Borrelia. I read this report, and although not junk science, it is of little practical use until their procedures become more precise, IMO. They really don't have much of a clue.
Rule #1 - whenever you see the word “antibodies” the research is most probably suspect.
..Trevor..
Molecualar survival strategies of the Lyme disease spirochete Borrelia burgdorferi Invasion of human neuronal and glial cells by an infectious strain of Borrelia burgdorferi
There are essentially two types of Lyme disease.
| acute Lyme disease | chronic Lyme disease | |
|---|---|---|
| Synonyms | early Lyme disease, acute Borelliosis | late Lyme disease, Post-Treatment Lyme Disease, Post–Lyme Disease Syndrome, chronic Borelliosis |
| Timing | Occurs days to weeks after the bite of an infected tick. | By some, thought to occur months to years after initial infection. |
| Conventional explanation for cause | A tick-borne disease, caused by at least three species of bacteria belonging to the genus Borrelia | Variable and highly controversial. Some argue chronic Lyme is psychosomatic. |
| Laboratory tests | A two-tiered protocol is recommended by the CDC for evaluation of the presence of Borrelia: the sensitive ELISA test is performed first, and if it is positive or equivocal, then the more specific Western blot is run. | Variety of (expensive) tests, none of which are widely accepted by the vast majority of mainstream researchers or physicians. The CDC and FDA issued a warning about “commercial laboratories that conduct testing for Lyme disease by using assays whose accuracy and clinical usefulness have not been adequately established. |
| Diagnosis | Diagnosed clinically based on symptoms, objective physical findings – such as erythema migrans (bulls eye rash), facial palsy or arthritis – or a history of possible exposure to infected ticks, as well as blood tests. Living in a tick-endemic area increases the likelihood of a Lyme diagnosis. | For those with a negative test for Borrelia, getting a diagnosis of chronic Lyme depends largely on whether the doctor is “Lyme literate”, that is if he/she even acknowledges the existence of chronic Lyme. |
| Controversy over legitimacy of diagnosis | Some disagreement over validity of tests, but controversy is relatively minimal. | Diagnosis is most controversially applied to patients with nonspecific symptoms (e.g., fatigue), who show no objective evidence they have been infected with Lyme disease in the past, since the standard diagnostic tests for infection are negative. Most physicians do not accept chronic Lyme as a legitimate diagnosis. |
| Treatment | Widely believed to be “readily curable.” Conventional approach according to 2008 Infectious Diseases Society of America guidelines24) – antibiotics of choice are doxycycline (in adults), amoxicillin (in children), erythromycin (for pregnant women) and ceftriaxone | “Lyme-literate” MDs often prescribe high-dose, often intravenous antibiotics such as Rocephin |
- Mental neurological symptoms - managing neurological symptoms
Tranmission Myths
Fear, ignorance and Internet rumors have also created an environment for expanding the mythology of Lyme's protean properties far beyond scientific fact or medical observation. For example, some Internet postings and websites suggest that Lyme can be acquired through sexual contact.
“I think that Lyme is also a STD [sexual-transmitted disease],” said one newsgroup poster. Another wrote, “I've talked to many couples who claim they transmitted to each other through sexual contact. I believe I gave it to my wife.”
At least a few LLMD appear to be telling patients that Lyme is sexually transmitted and therefore their family members should be tested. One person reported to Quackwatch that a family member had been tested and told that the test was positive and that a 4-5 month course of antibiotics was necessary.
There is no basis for such advice or beliefs. Lyme infections are acquired from the bite of an infected tick. People are “dead end” hosts and do not spread Lyme infections to others.
Lyme does not culture easily
While I understand that the material in this release may sound earth-shattering to folks who have come in contact with only the traditional view of Lyme disease, the material here is still not up-to-date, and is very limited in its outlook.
I do understand pretty well what the issues are here, and I have tried several times to communicate them to the MP membership.
The problem is that the Lyme genome is not homogenous, despite what the 'experts' would have you believe. There is a chromosome with about 500,000 bp and 21 linear and circular plasmids with nearly as many genes on them as are on the chromosome. Each plasmid is mobile and self-replicating. So it is in fact stupid (IMO) to keep talking about Borrelia as one species. It is not one species. It is not even close to being one species. It is not even clear how much of the genome is necessary to create a viable spirochete, let alone viable L-formsDifficult-to-culture bacteria that lack a cell wall and are not detectable by traditional culturing processes. Sometimes referred to as cell wall deficient bacteria.. So to talk about variations in sub-species is missing the point. Please, first define the species itself, then talk about sub-species variation. The same goes (to a lesser degree) for Treponema and Rickettsia.
Some sarcoidosis and CFS patients have no borrelia-specific markers. Clearly, borrelia is not the only organism involved in Th1 disease.
But those who understand these pathogens (at the detailed level of their genome) cannot yet communicate with the clinicians who are out in the field, and who get to speak to the press. We speak a different language.
How many of the sources quoted in this article would even know what a plasmid is? That is the problem that patients face. The genome has brought a revolution in knowledge about pathogenic species that only a fraction of the medical community (less than 1%) are equipped to understand. In general, patients will have to wait at least a decade for any of the concepts about these diseases to change - wait until either 'Continuing Medical Education' gets given teeth, or a new generation of clinicians comes into the workforce.
Thanks for posting this article anyway, I guess it gives us the chance to discuss the real issues.
~Trevor Marshall, PhD
Is Lyme disease always poly microbial?-The jigsaw hypothesis 13
Abstract: Lyme disease is considered to be caused by Borrelia species of bacteria but slowly evidence is accumulating which suggests that Lyme disease is a far more complex condition than Borreliosis alone. This hypothesis suggests that it may be more appropriate to regard Lyme disease as a tick borne disease complex. Over recent years numerous different microbes have been found in ticks which are known to be zoonotic and can coinfect the human host. The hypothesis suggests that multiple coinfections are invariably present in the clinical syndromes associated with Lyme disease and it is suggested that these act synergistically in complex ways. It may be that patterns of coinfection and host factors are the main determinants of the variable clinical features of Lyme disease rather than Borrelia types. An analogy with a jigsaw puzzle is presented with pieces representing Borreliae, coinfections and host factors. It is suggested that many pieces of the puzzle are missing and our knowledge of how the pieces fit together is rudimentary. It is hoped that the hypothesis will help our understanding of this complex, enigmatic condition.
It may be that patterns of coinfection and host factors are the main determinants of the variable clinical features of Lyme disease rather than Borrelia types. An analogy with a jigsaw puzzle is presented with pieces representing Borreliae, coinfections and host factors. It is suggested that many pieces of the puzzle are missing and our knowledge of how the pieces fit together is rudimentary. It is hoped that the hypothesis will help our understanding of this complex, enigmatic condition.
Trevor also stated, “In my opinion it is likely that Borrelia burgdorferi sensu stricto is not a homogenous organism, is not a homogenous genome.”
Question: Trevor asked, “…so why are we elevating Borrelia to status as the primary pathogen?”
Question: Can borrelia change from spirochete to coccoid to L-forms?
Oct. 7, 2005: The problem is actually a lot more complex than it seems. The genome of Borrelia has about 40% of its genes on mobile plasmids, and not on the primary chromosome. So (arguably) there could be hundreds of different versions of B.burgdorferi out there.
If you look at the master genome list at 820 Complete Microbial Genomes you will find only two Borrelia species fully sequenced. One was sequenced by TIGR and one from Germany. Look at the sizes - 1.52 vs 0.99. This is because the Germans are only reporting the Chromosome and 2 plasmids, while TIGR is reporting chromosome and 21 plasmids.
Unfortunately the Borrelia genome has proven too complex for many of our institutions to fully assimilate, and this is an excellent example. Both groups are correct, but they are looking at the species in different ways.
A similar situation exists within the Mycoplasma species. Look for example, at this species comparison: Gene map of the Mycoplasma pneumoniae genome
The rapid pace of advance in science's knowledge of the genome has left 99.9% of our infectious diseases specialists behind. It will take a new generation to come along who can understand the new genomic tools.
~Trevor Marshall, PhD
This is a fascinating critique of Lyme Disease advocacy which has sent the Lyme community into a frenzy. The strange thing is, I find it hard to refute the basic thrust of the article, there really is little or no science supporting the persistence of Borrelia burgdorferi. As the article details, the tests promoted by the community are in fact not properly validated or properly interpreted and the tendency to call all diagnoses “Lyme Disease” seems scientific imprecision at its worst. I am not saying that Borrelia spp is not a persistent pathogen, I am saying that any science given to support the assertions of the Lyme community is very weak. Which is the thrust of this article.
We need to make sure that we do not fall into the same trap with the MP, and indeed, for many years I have taken the Lyme and CFS communities as a model of exactly how we should not drive the MP forward.
We have to walk a fine line here.
Trevor
References
[PMID: 17928580] [DOI: 10.1212/01.WNL.0000284604.61160.2d]
[PMID: 17928578] [DOI: 10.1212/01.WNL.0000291407.40667.69]
[PMID: 17587070] [DOI: 10.1007/s10096-007-0340-2]
[PMID: 21383843] [PMCID: 3044169] [DOI: 10.1371/journal.pone.0017287]
[PMID: 335422]
[PMID: 11448704] [DOI: 10.1016/s0022-3999(01)00223-9]
[PMID: 10375340] [DOI: 10.7326/0003-4819-130-11-199906010-00016]
[PMID: 19855350]

